Why are CYP enzymes a key focus for liver disease research?
Published on: 13 Jan 2020
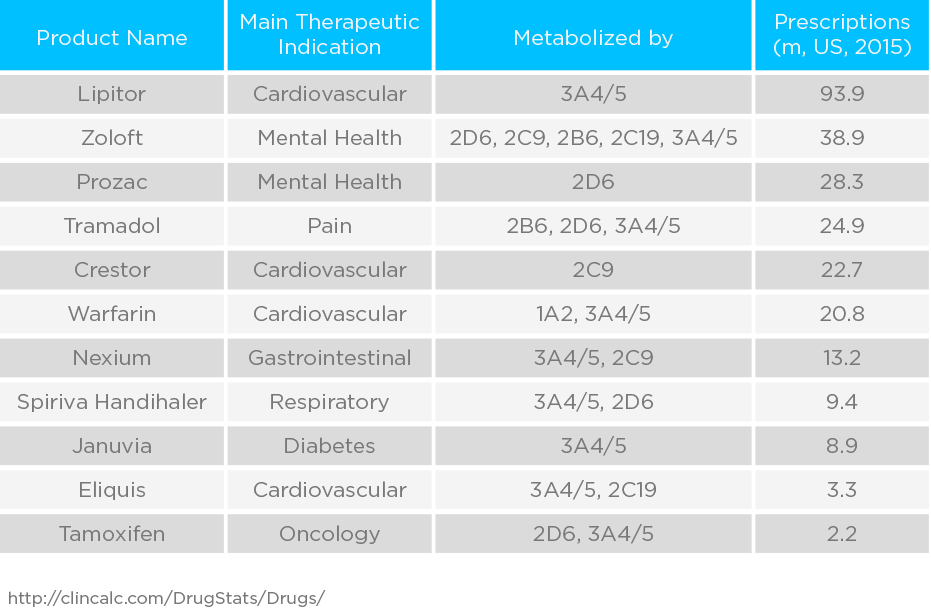
Cytochrome P450 (CYP450) proteins are a family of approximately 60 different enzymes in humans. These enzymes account for 70 to 80 percent of drug metabolism. The CYP450 proteins are expressed mainly in the liver and gut mucosa, where they oxidize steroids, fatty acids, and xenobiotics, and are important for the clearance of various compounds from the bloodstream, as well as for hormone synthesis and breakdown1.
The high expression levels in the hepatic tissue, make CYP450 enzymes excellent targets for diagnostic purposes because their activity changes in liver disease. Furthermore, genetic alterations of CYP450 in certain individuals result in isoforms able to metabolize drugs faster or slower compared to the general population. Therefore, knowledge of these isoforms in each individual is key to identifying optimal drug dosage and minimize the possibility of adverse drug reactions due to overdosage or drugs interactions.
Approaches to Studying CYP450 Enzymes
There are currently three different approaches for investigating the activity of cytochromes. However, these methods have limitations and require invasive sampling:
- Purified proteins – Incubating a purified protein and the candidate substrate together in isolation to measure the level of substrates and products after a given time. This method can only be used to only test one enzyme at a time and takes it out of its natural biological context.
- Microsomes – Retrieving CYP450 microsomes from the liver, adding the substrate and measuring the production of products. The quality of microsome recovery can vary depeding on the experimental approach and results can easily be confounded due to contaminants.
- In vivo – Administering drugs to patients and measuring cytochrome activity via a drug washout, measured via blood sampling. There are many confounding factors when studying individual enzymes within a patient, inability to properly control conditions makes it challenging to acquire clear results.
The EVOC® Probe Approach
A new non-invasive approach, EVOC® Probes, could change the way we study enzyme activity by collecting and analyzing breath samples. An EVOC Probe containing substrates for relevant cytochromes can be safely administered to a patient and metabolized in the body, resulting in products that are excreted in the breath. This approach enables high levels of safe compounds to be administered, such that fold changes in levels are much more visible, with substantially improved signal-to-noise ratios over those that come from endogenous sources.
EVOC Probes have the potential to produce a clear and unambiguous measure of liver function, and to distinguish between the different types of liver disease from the activity of the key liver enzymes. This can be achieved by measuring the levels of the substrate in the EVOC Probe and its metabolites.
Limonene: An Exogenous Breath Biomarker for Liver Metabolism?
Limonene is not produced by the body, but is ingested due to its presence in many foods and drinks. Inside the body it is metabolized by the CYP450 enzymes CYP2C9 and CYP2C19 to perillyl alcohol, trans-carveol and trans-isopiperitenol2. Levels of the CYP2C19 enzyme have been found to be reduced in patients with cirrhosis, and that inversely correlates with disease severity3. As a result of these enzymatic changes, Fernández del Rio et al. reported elevated limonene levels in the breath of patients with cirrhosis compared to controls4, suggesting that a breath test for limonene could be developed as a test to detect and assess the severity of liver cirrhosis.
These existing studies measured breath limonene without taking into account exposure through diet, pharmaceuticals, or environment, reducing the sensitivity of the resulting models. In the EVOC Probe method, we seek to control the limonene dose for each patient and increase the concentration of breath limonene by administering a known quantity of limonene before testing, resulting in more reliable and precise results.
Share your views on breath biomarkers for liver disease on the Breath Biopsy Community.
Identifying Further Enzymes and Pathways
While limonene provides one example of what EVOC Probes can achieve in liver disease, there’s a need to determine further examples. The initial challenge is to find pathways that we can test with probes detectable in the breath. We are seeking to identify a panel of pathways that will enable us to diagnose and monitor the progression of liver disease by measuring enzyme activities.
EVOC Probes offer the opportunity to clearly and independently monitor several enzymes in parallel and use these as a comprehensive read-out of liver health that could give clear indicators of disease progression. For example, in early liver disease, mitochondrial activity is affected resulting in an increased beta-oxidation rate5. This is due to the alteration of the electron transport chain and/or oxidative phosphorylation leading to inappropriate oxidative metabolism of substrates6. Elements of this pathway could be suitable for examination using EVOC Probes.
To learn more about breath limonene and liver disease, check out the webinar Dr. Giuseppe Ferrandino gave, discussing studies that have shown that cirrhotic patients have raised levels of limonene in their breath – a phenomenon observed because of the reduced liver capability to metabolize limonene, or visit our EVOC Probes page.
References:
- https://ghr.nlm.nih.gov/primer/genefamily/cytochromep450
- Miyazawa et al. (2002). Metabolism of (+)- and (-)-limonenes to respective carveols and perillyl alcohols by CYP2C9 and CYP2C19 in human liver microsomes. Drug Metab Dispos.; DOI: 10.1124/dmd.30.5.602
- Frye et al. (2006). Liver disease selectively modulates cytochrome P450-mediated metabolism. Clinical Pharmacology and Therapeutics.; DOI: 10.1016/j.clpt.2006.05.006
- Fernandez del Rio et al. (2015). Volatile Biomarkers in Breath Associated With Liver Cirrhosis — Comparisons of Pre- and Post-liver Transplant Breath Samples. EBio Med.; DOI: 10.1016/j.ebiom.2015.07.027
- Miele et al. (2003). Hepatic Mitochondrial Beta-Oxidation in Patients With Nonalcoholic Steatohepatitis Assessed by 13C-Octanoate Breath Test. The American J. of Gastro.; DOI: 10.1111/j.1572-0241.2003.07725.x
- Grattagiano et al. (2011). Mitochondria in Chronic Liver Disease. Current drug targets.; DOI: 10.2174/138945011795528877
Catch up on the presentations from the Breath Biopsy Conference 2024
