Respiratory Droplets
Collecting respiratory droplets exhaled as breath aerosols enables the collection of non-volatile biomarkers for analysis using a range of established analytical techniques
Respiratory Droplets Contain a Wide Array of Biomarkers
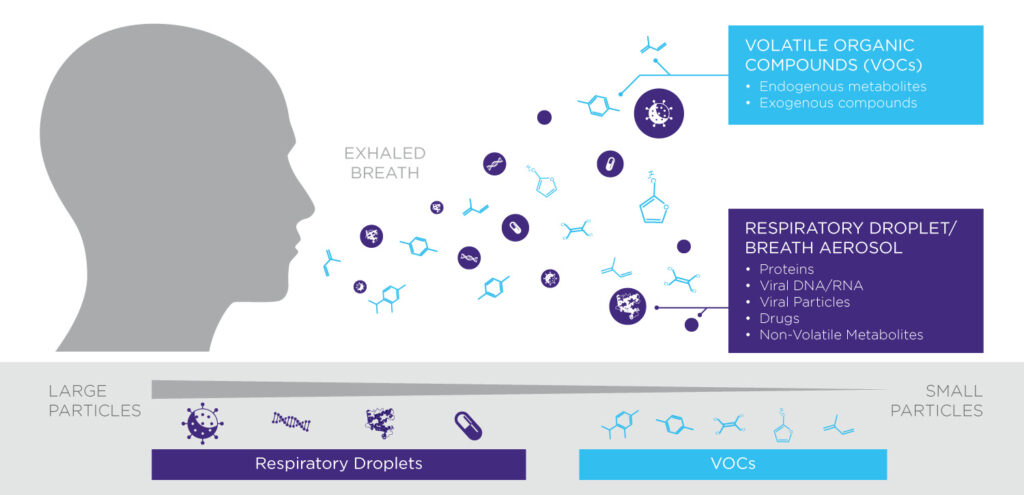
In addition to gases and volatile compounds, exhaled air is full of microscopic respiratory droplets, each less than 100 microns across. The contents of these respiratory droplets include non-volatiles, which can be useful biomarkers for the detection and treatment of disease.
Respiratory droplets are exhaled as breath aerosols, often studied as fine aerosols (<5 microns) and coarse aerosols (>5 microns). Each respiratory droplet can contain non-volatile metabolites, proteins, lipids, nucleotides and viral particles.
Why Collect Breath Aerosols?
Breath Biomarkers in respiratory droplets have many possible applications. Breath aerosol collection is used by sporting organisations for anti-doping testing [1-3] and can also be used to detect a range of illicit recreational drugs [4-6]. Respiratory droplets have demonstrated utility in identifying inflammation through the detection of cytokines and other immune signalling molecules. There is also evidence that respiratory droplets have application in infectious diseases using RNA or DNA as biomarkers for the presence of pathogens.
There are various advantages to collecting respiratory droplets as a source of biomarkers:
- It’s non-invasive and ensures patient comfort
- It’s cheap and easy to do anywhere
- It doesn’t require healthcare experience or specialist training
- It integrates seamlessly with a wide range of established analysis workflows
Origins of Respiratory Droplets
Biomarkers in breath aerosols are of particular interest because they are generated in the deep airways of the lungs [7,8], close to where gas exchange occurs and where several severe lung infections reside.
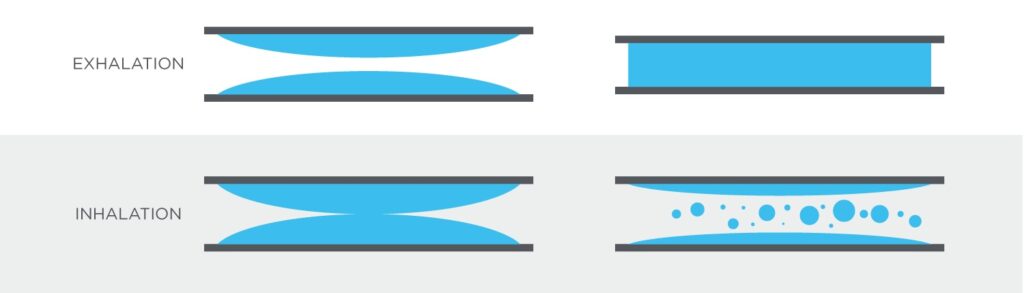
Respiratory droplets are thought to be formed through a process called bronchiole fluid film burst (BFFB) caused by the closure and reopening of lower bronchioles during regular breathing [9]. The airways of the lungs are lined with fluids containing surfactants, which lower the surface tension. Towards the end of exhalation, these fluids can form films across smaller airways. As bronchioles open again during inhalation, these fluid films burst releasing respiratory droplets as aerosol particles that are drawn into the alveoli and then expelled on the next exhalation. Production of respiratory droplets in breath aerosols can be increased through deep exhalation and rapid inhalation.
Uses for Respiratory Droplets
The diversity of particles that can be captured and analyzed from respiratory droplets means that they have a wide range of potential applications. They have already found some value in anti-doping for competitive sports, where drugs such as steroids, hormone treatments and stimulants can be collected and directly identified through liquid chromatography mass spectrometry (LC-MS) approaches. Similar applications have been explored for the detection of amphetamines, THC etc. as markers of drug abuse. Other uses being investigated include detection of inflammation, particularly linked to lung damage, identification of environmental exposures and the detection of pathogens, particularly respiratory viruses such as influenza.
The collection and analysis of exhaled breath aerosols is still a developing field and there are many potential applications that have yet to be explored, get in contact to find out more.
References
- Thevis et al. (2016) Sports drug testing using complementary matrices: Advantages and limitations. J Pharm Biomed Anal. ;130:220-230. doi: 10.1016/j.jpba.2016.03.055
- Bowers & Bigard (2017) Achievements and Challenges in Anti-Doping Research. Med Sport Sci. ;62:77-90. doi: 10.1159/000460702.
- Thevis et al. (2017) Expanding analytical options in sports drug testing: Mass spectrometric detection of prohibited substances in exhaled breath. Rapid Commun. Mass. Spectrom. ;31:1290-1296. doi: 10.1002/rcm.7903
- Arvidsson et al. (2019) Drug abuse screening with exhaled breath and oral fluid in adults with substance use disorder. Drug Test Anal. ;11(1):27-32. doi: 10.1002/dta.2384
- Ullah et al. (2018) A liquid chromatography and tandem mass spectrometry method to determine 28 non-volatile drugs of abuse in exhaled breath. J Pharm Biomed Anal. ;148:251-258. doi: 10.1016/j.jpba.2017
- Ljungkvist et al. (2017) Two techniques to sample non-volatiles in breath-exemplified by methadone. J Breath Res. ;12(1):016011. doi: 10.1088/1752-7163/aa8b25
- Gebhart et al. (1988) The Human Lung as Aerosol Generator. J. Aerosol Med. ;1:196-7.
- Effros et al. (2005) Epithelial lining fluid solute concentrations in chronic obstructive lung disease patients and normal subjects. J Appl Physiol (1985).;99(4):1286-92. doi: 10.1152/japplphysiol.00362.2005
- Johnson et al. (2009) The mechanism of breath aerosol formation. J Aerosol Med Pulm Drug Deliv. ;22(3):229-37. doi: 10.1089/jamp.2008.0720