The Origins of Isoprene in Human Breath
Unique gene mutations in individuals lacking breath isoprene suggest links to muscular metabolism.
| Publication Information: Sukul P, Richter A, Junghanss C, Schubert JK, Miekisch W. Origin of breath isoprene in humans is revealed via multi-omic investigations. Commun Biol. 2023 Sep 30;6(1):999. doi: 10.1038/s42003-023-05384-y
Disease Area: Musculoskeletal metabolism. Application: Breath analysis is used to determine levels of isoprene in participants. Individuals lacking breath isoprene were identified as having a mutated IDI2 protein, an enzyme that catalyzes the production of cholesterol. Sample medium: Breath Analysis approach: PTR-ToF-MS Summary: This study on isoprene and the metabolic pathways of isoprene production found unique gene mutations in individuals lacking isoprene. Results suggest its link to muscular metabolism, musculoskeletal medicine and exercise science and could lead to its clinical translation as a biomarker. |
Isoprene, or 2-methyl-1,3-butadiene, is a volatile organic compound (VOC) endogenously produced in both plants and animals for the synthesis of steroid hormones and terpenoids. Long established as one of the major VOCs exhaled in human breath (1), isoprene has been proposed as a potential biomarker for a range of diseases, including cancers and heart failure (2,3). Isoprene levels in exhaled breath have also been demonstrated to increase in response to exercise, as seen in a recent study which identified a significant increase in isoprene levels between pre- and post-race breath samples taken from ultramarathon runners
Isoprene has widely been suggested to be related to cholesterol biosynthesis, but a precise origin of production has not been defined. The liver has previously been claimed to be the major site for cholesterol synthesis resulting in isoprene entering breath using pre-clinical data, but little evidence from clinical trials has supported this proposal. For instance, King et al. presented data based on physiological modeling of variability of isoprene levels in exercise that indicated an extrahepatic source of endogenous isoprene (5). The lack of a known metabolic origin for breath isoprene is a major contributing factor to the prevention of its clinical translation.
A 2023 study by Sukul et al. investigating the metabolic origin of breath isoprene was conceived after investigations into the dynamic nature of exhaled VOCs under varying metabolic and physiological effects revealed a participant who displayed no isoprene detectable in breath (6). It was then determined that the participant’s parents and sister were also isoprene deficient, prompting a wider study to identify further adults lacking breath isoprene. These findings provided the possibility to identify the origin of isoprene within humans, a first step towards isoprene’s application as a clinically translatable biomarker by eliminating speculation over its origin and function.
Identifying the origin of isoprene in humans
As seen in Figure 1, the study measured the isoprene levels in the breath of 2000 participants and determined whether the participants had normal, deficient, or absent levels of isoprene. Five rare cases of isoprene absence were identified (3 females and 2 males). The 5 isoprene-absent participants were invited back for further multi-omics investigations, including whole exome sequencing, breathomics, and serological analyses, to identify differences with the normal healthy population that may relate to the absence of isoprene. No serological aberration was found in the isoprene-absent adults and all other exhaled endogenous VOCs were found to be within the expected range. A series of filtering strategies were used to find candidate mutations shared by the isoprene-absent participants, leading to the isopentenyl-diphosphate delta isomerase-2 (IDI2) stop-gain mutation being identified as a shared feature.
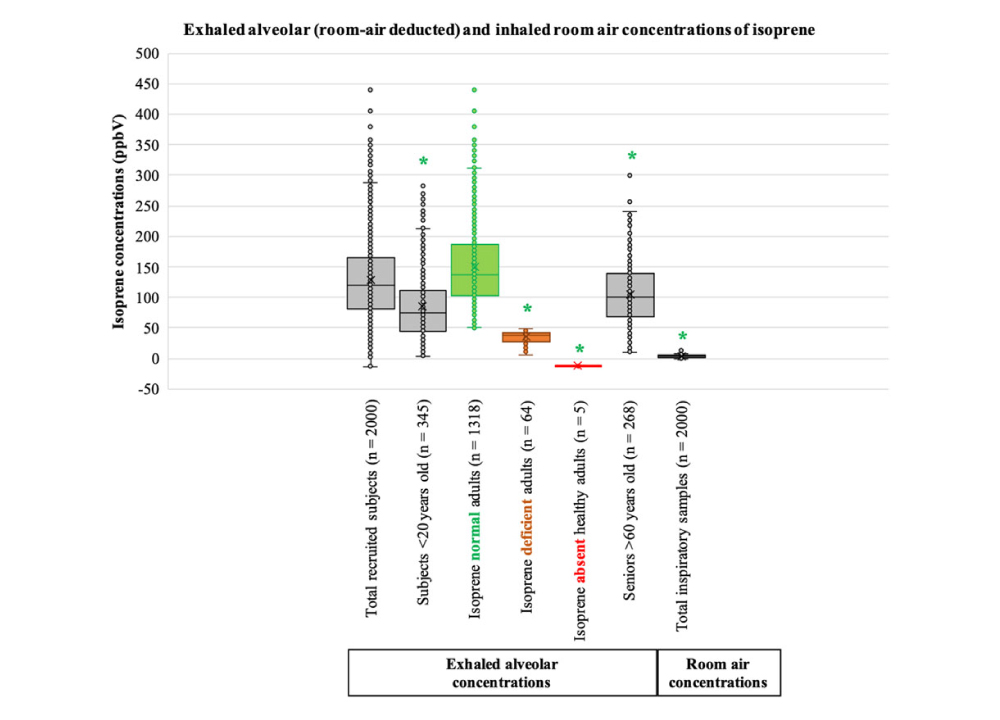
Figure 1: Distribution of exhaled alveolar and inhaled room air concentrations of isoprene. Distribution of isoprene concentrations from exhaled alveolar and inhaled room air samples. The graph represents isoprene concentrations (ppbV) on its y-axis. The x-axis divides the total number of recruitments into different subgroups for age and the levels of isoprene on exhaled breath, as well as the total number of inspiratory samples. The age categories represented are below 20 years, 20-60 years and above 60 years, with the 20-60 years category grouped into normal isoprene (exhaled isoprene concentrations >50 ppbV), isoprene deficient (exhaled isoprene concentrations <50 ppbV) and isoprene absent healthy. A green-colored ‘*’ has been used to represent statistically significant differences in comparison to ‘isoprene normal adults’. The statistically significant differences were determined using pairwise-multiple comparisons of one-way ANOVA on ranks (p-value ≤ 0.005). Figure from Sukul et al. 2023 (6).
IDI2 is an enzyme with muscle-specific expression that catalyzes the production of cholesterol from a precursor molecule (7,8). The IDI2 mutation identified as unique to isoprene-absent individuals causes the truncation of the mRNA molecule, resulting in the loss of the second enzymatic site on the protein and subsequently impaired or absent protein function. The loss of the c-terminal region of the enzyme caused by the mutation also deletes two of the four magnesium ion binding sites, preventing the association of the co-factor required for enzyme function. Bottle-nose dolphins have previously been identified as mammals that do not exhale isoprene, and further investigation revealed that dolphins do not express IDI2 (9) – strengthening the link between the function of the IDI2 enzyme to presence of isoprene in the breath.
Discussion and conclusions
The finding that functional IDI2 expression as a contributor to the human breath isoprene indicates that isoprene expression may be related to muscular metabolic activity, as demonstrated in the pathway displayed in Figure 2 below, rather than being of hepatic origin. Muscle movement and activity cause increased breath isoprene levels, suggesting that the compound may be originating from lipolysis in skeletal muscle, particularly as wild-type IDI2 acts as a rate-limiting factor for its endogenous production.
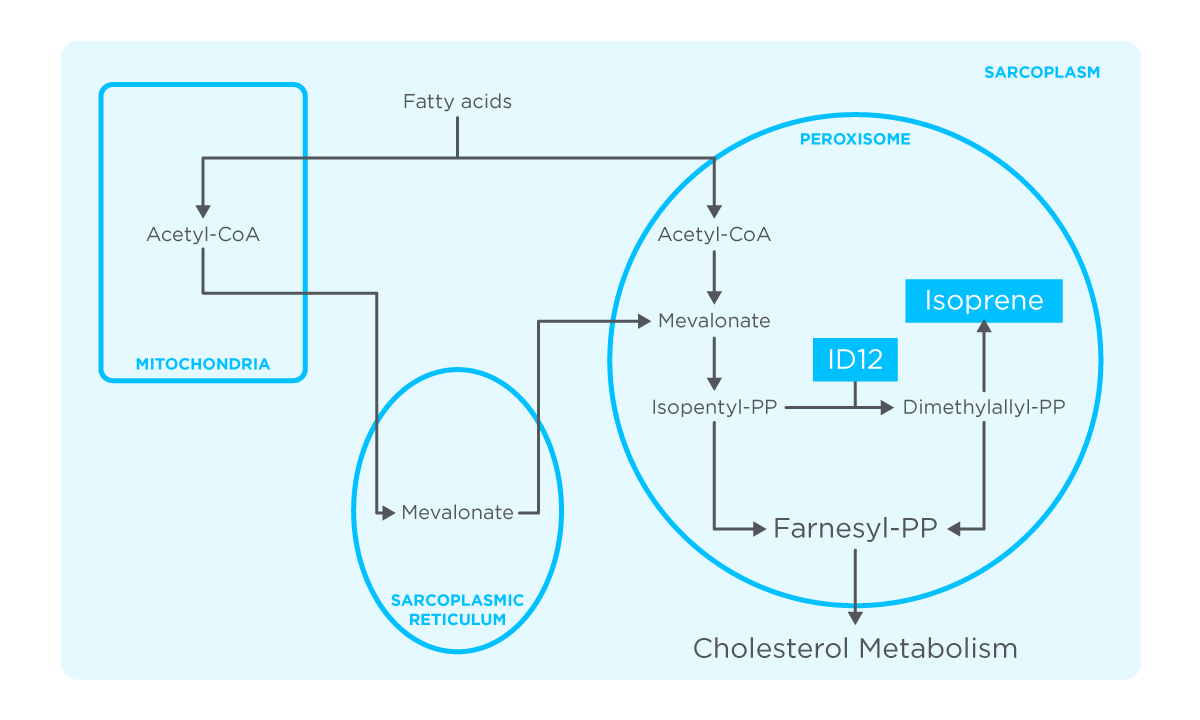
Figure 2: Metabolic pathway of isoprene production in human skeletal-myocyte. Figure based on results from study by Sukul et al. 2023 (6). The mitochondria, sarcoplasmic reticulum, sarcoplasm and peroxisome are all organelles proposed to contribute to this pathway. The peroxisomes, metabolic organelles largely responsible for lipolysis, are proposed to be the major site of isoprene production, with human IDI2 expressed highly here. The beta-oxidation of fatty acids to acetyl-coA occurs in the mitochondria and peroxisome, followed by conversion to mevalonate, which can take place in the sarcoplasmic reticulum. Mevalonate is then converted to isopentyl-PP (IPP), which is then converted into its active isoform dimethylallyl-PP (DMAPP) by IDI2 activity. DMAPP is then used to produce isoprene. Farnesyl-PP can be produced by IPP and DMAPP before use in other metabolic pathways, such as cholesterol metabolism.
Further investigations into the expression of isoprene in individuals with, for instance, muscle dystrophy or various exercise training regimes could potentially reveal more about these aspects of muscle metabolism. Research into the upstream cascades of these metabolic pathways and the relationship between isoprene expression and IDI2 genotype should also take center focus to gain a deeper understanding of the isoprene production pathway in humans. Further defining the origins and pathways of isoprene production is essential if isoprene is to be used as a routine clinical biomarker.
As isoprene has been strongly implicated in the musculoskeletal system, it should be brought into consideration as a potential biomarker within musculoskeletal medicine, potentially in relation to sports and exercise science, for example in monitoring athlete health. Isoprene exhalation has also been shown to have endocrine regulation and ageing dependency, meaning investigations into isoprene in ageing, muscle mass development and related conditions may also be appropriate. Owlstone Medical’s Breath Biopsy technology, isoprene has already been identified as a key component that changes in the breath of ultra-marathon runners in pre- and post-race samples, furthering the relationship of isoprene expression and muscle activity (4).
Knowledge of the origins of VOCs within the body is essential for the correct clinical interpretations of endogenous biomarkers. Increasing this knowledge could vastly increase the number of breath biomarkers available for usage in a clinical setting, as hundreds of different VOCs exhaled in the breath have already been identified and characterised in our Breath Biopsy Atlas, with some needing more investigation to understand their biological functions and origins. To find out more about our VOC Atlas and Breath Biopsy technology, follow the links below to get in contact with us.
References:
- Gelmont D, Stein RA, Mead JF. Isoprene-the main hydrocarbon in human breath. Biochem Biophys Res Commun. 1981 Apr 30;99(4):1456-60. doi: 10.1016/0006-291x(81)90782-8.
- Fuchs D, Jamnig H, Heininger P, Klieber M, Schroecksnadel S, Fiegl M, Hackl M, Denz H, Amann A. Decline of exhaled isoprene in lung cancer patients correlates with immune activation. J Breath Res. 2012 Jun;6(2):027101. doi: 10.1088/1752-7155/6/2/027101.
- McGrath LT, Patrick R, Silke B. Breath isoprene in patients with heart failure. Eur J Heart Fail. 2001 Aug;3(4):423-7. doi: 10.1016/s1388-9842(01)00128-3.
- Chou H, Arthur K, Shaw E, Schaber C, Boyle B, Allsworth M, et al. Metabolic insights at the finish line: deciphering physiological changes in ultramarathon runners through breath VOC analysis. J Breath Res. 2024 Apr 1;18(2):026008. doi: 10.1088/1752-7163/ad23f5
- King J, Koc H, Unterkofler K, Mochalski P, Kupferthaler A, Teschl G, Teschl S, Hinterhuber H, Amann A. Physiological modeling of isoprene dynamics in exhaled breath. J Theor Biol. 2010 Dec 21;267(4):626-37. doi: 10.1016/j.jtbi.2010.09.028.
- Sukul P, Richter A, Junghanss C, Schubert JK, Miekisch W. Origin of breath isoprene in humans is revealed via multi-omic investigations. Commun Biol. 2023 Sep 30;6(1):999. doi: 10.1038/s42003-023-05384-y.
- PubChem. IDI2 – isopentenyl-diphosphate delta isomerase 2 (human) [Internet]. [cited 2024 Feb 20]. Available from: https://pubchem.ncbi.nlm.nih.gov/gene/IDI2/human
- IDI2 – Isopentenyl-diphosphate delta-isomerase 2 – Homo sapiens (Human) | UniProtKB | UniProt [Internet]. [cited 2024 Feb 20]. Available from: https://www.uniprot.org/uniprotkb/Q9BXS1/entry#expression
- Aksenov AA, Yeates L, Pasamontes A, Siebe C, Zrodnikov Y, Simmons J, McCartney MM, Deplanque JP, Wells RS, Davis CE. Metabolite content profiling of bottlenose dolphin exhaled breath. Anal Chem. 2014 Nov 4;86(21):10616-24. doi: 10.1021/ac5024217.