Stratifying asthma patients using just four exhaled VOCs
Published on: 9 May 2019
A study involving over 500 asthma patients published in Analytical Chemistry shows that analysis of just four volatile organic compounds (VOCs) in exhaled breath can be used to effectively discriminate between inflammatory asthma phenotypes with statistical accuracy comparable to more complex and invasive methods.
Asthma is a broad spectrum of conditions defined by chronic inflammation in the airways of the lungs. This inflammation has various origins and triggers and encompasses a range of phenotypes and pathophysiologies. As such, treatment strategies can vary greatly from patient to patient. One of the main distinctions between asthma cases is the type of immune cells involved in causing inflammation. Cases that are primarily eosinophilic typically respond well to glucocorticoid steroid treatments. By contrast, cases dominated by neutrophils show a poor response to steroids (Find out more in our Asthma case study).
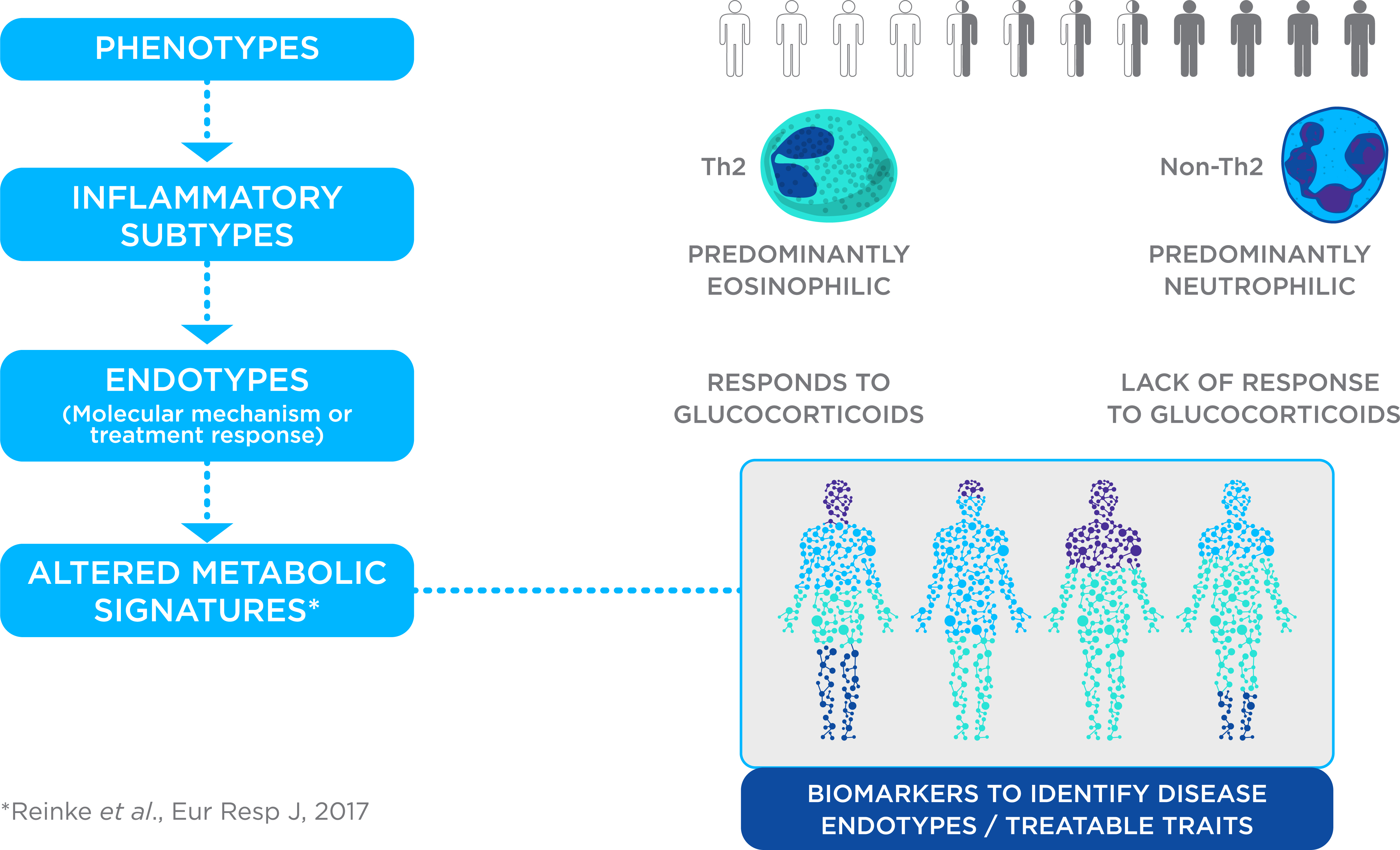
The cellular and molecular make-ups of different asthma phenotypes suggest that cases could be distinguished on the basis of their metabolic signatures. As such, it may be possible to use VOCs in exhaled breath to stratify asthma patients. This may permit a precision medicine approach to asthma treatment where treatment strategies can take account of the biological characteristics of each case.
A previous in vitro study of asthma cell pathologies identified a selection of VOCs that could distinguish cell cultures from eosinophilic and neutrophilic asthmas in culture. In a continuation of this work, Schleich et al. have now demonstrated comparable results using exhaled VOC samples in vivo.
Our study is the first attempt to characterize VOCs according to sputum granulocytic profiles [inflammation subtype] in a large population of asthmatics.
Four VOCs help to identify eosinophilic and neutrophilic asthmas
In total, Schleich et al. collected samples from over 500 asthma patients including a discovery study of 276 patients and a validation study with 245. All patients were recruited and sampled at the same site in Liege, Belgium. Patients were associated with asthma types on the basis of induced sputum testing – currently the best method for asthma stratification. Compared to collecting exhaled VOCs, induced sputum sampling is time-consuming, complex, and unsuitable for various patient situations.
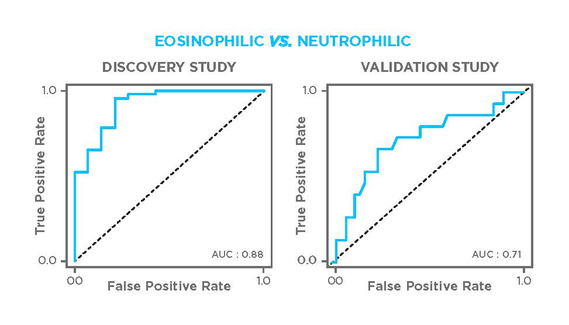
Throughout, data from the discovery study was used to identify relevant VOCs and to develop predictive algorithms based on those results. As such, the results of applying the algorithms to data from the discovery study are expected to be high. In the validation study, the same algorithms were applied to a biologically distinct set of data to test how adaptable and robust the models are for different populations. Achieving high-quality results in the validation study is the real test of a quality diagnostic approach.
The discovery study used GC-MS analysis to identify suitable VOCs, while the replication study applied GCxGC-HRTOFMS to detect the selected VOCs. Schleich et al. identified four VOCs as key discriminants of asthma types. Patients with neutrophilic asthmas exhaled elevated levels of nonanal, 1-propanol, and hexane relative to other phenotypes, while eosinophilic asthmas could be characterized by lower levels of hexane and 2-hexanone.
In both the discovery and validation studies, also nonanal proved to be a key predictor for direct discrimination of eosinophil vs. neutrophil phenotypes. The discovery model, which also included 3,7-dimethylnonane and 1-propanol, achieved 70% accuracy, 45% sensitivity, and 85% specificity with an area under receiver operating characteristic curve (AUROC) of 0.88.
In comparison to other methods
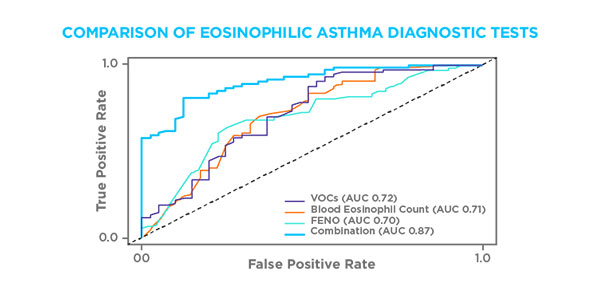
Previous studies have also shown that exhaled NO gas (FeNO) and blood eosinophil levels can be key indicators of eosinophilic asthma. Schleich et al. compared VOC measurement to a model that combined FeNO and blood eosinophil readings and found that both approaches give comparable accuracies, with VOC giving an overall better balance of sensitivity and specificity. Furthermore, combining all three readings enabled the team to achieve an AUROC of 0.87 (accuracy 76%, sensitivity 79%, specificity 78%) in the replicate cohort.
By contrast, neutrophilic asthma has proven much more difficult to test for reliably and there is a lack of established biomarkers for this condition. This study used nonanal, 1-propanol, and hexane to distinguish neutrophilic asthma with an AUROC of 0.73 (76% accuracy, 81% sensitivity, and 43% specificity). This is comparable to the statistical power of the predictors mentioned above for eosinophilic asthma i.e. FeNO or blood eosinophils. However, when the VOC data were combined with preselection on the basis of neutrophil sputum testing they achieved an AUROC of 0.97 (sensitivity 71%, specificity 100%).
Confounding factors
The study examined the effects of age on VOCs – particularly as the number of neutrophils in sputum is known to increase with age – and found no connection. The team also examined the replication population to see if the four identified VOCs were affected by smoking. They weren’t able to distinguish smokers, ex-smokers, and non-smokers using these VOCs. These VOCs also couldn’t be used to identify whether or not patients have had access to steroid treatments for their asthma.
This suggests that these four VOCs provide a relatively reliable and robust basis for the stratification of asthma patients in a way that is not affected by likely confounding factors of age, smoking habits, and prior treatments.
Outcomes
Schleich et al. have demonstrated the power of a relatively small number of VOCs to effectively and non-invasively stratify asthma patients in a manner that could be applied as a means to diagnose patients and develop treatment strategies. There are still issues to address, particularly in examining how well this system copes with a more varied population of asthma patients from different locations. These studies also don’t help to reveal the origins of these VOCs in asthma and how or why they occur to different extents in different forms of the condition. Yet this is an important step toward the use of breath analysis in the diagnosis and treatment of asthma worldwide.
Reference
Florence N Schleich, Delphine Zanella, Pierre-Hugues Stefanuto, Kirill Bessonov, Agnieska Smolinska, Jan W Dallinga, Monique Henket, Virginie Paulus, Françoise Guissard, Sophie Graff, Catherine Moermans, Emiel F. M. Wouters, Kristel Van Steen, Frederik-Jan van Schooten, Jean-François Focant, and Renaud Louis (2019) Exhaled Volatile Organic Compounds are Able to Discriminate between Neutrophilic and Eosinophilic Asthma, Am J Respir Crit Care Med, doi.org/10.1164/rccm.201811-2210OC