Why should we study liver diseases using breath analysis?
Published on: 4 Oct 2019
The NHS has reported an increase in liver disease in people under 75 and currently 75% of diagnoses [1] occur at a late stage, meaning treatment through lifestyle changes is not possible and the cost of treatment increases dramatically. The key to preventing deaths and reducing the costs of treatment is earlier detection and intervention – The British Liver Trust indicate that 90% of liver disease is preventable through early detection and survival of patients increases with early diagnosis [2].
The costs of treating liver disease are high, with the US Center for Disease Analysis estimating a spend of $5billion annually in health-care treating the disease [3]. This includes organ transplants, inpatient hospitalization and outpatient appointments, diagnosis, procedures and medication. Data also indicates that liver disease is a significant financial burden to healthcare providers in Europe [4], with the importance of early diagnosis and treatment highlighted for non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH).
A lack of identifiable symptoms makes early detection of liver disease difficult [5]. Once symptoms present, the liver is often already irreparably damaged and scarred. Therefore if diagnosis happens in the early stages it is often incidental due to patients having blood tests, ultrasounds, CT scans, MRIs or tissue biopsies for other purposes. The time consuming and often extremely invasive nature of these procedures can be a further limiting factor in early diagnosis of liver diseases.
A non-invasive test for liver disease, for example based on breath testing, could enable general screening of the population, greatly reducing the costs associated with these conditions.
In a previous blog we outlined the story so far in regards to liver disease and diagnosis via non-invasive breath analysis. The liver is vital to many of the key metabolic processes within the body and the products of these processes have the potential to be studied as biomarkers to measure and monitor the function of the liver and to identify early indicators of disease.
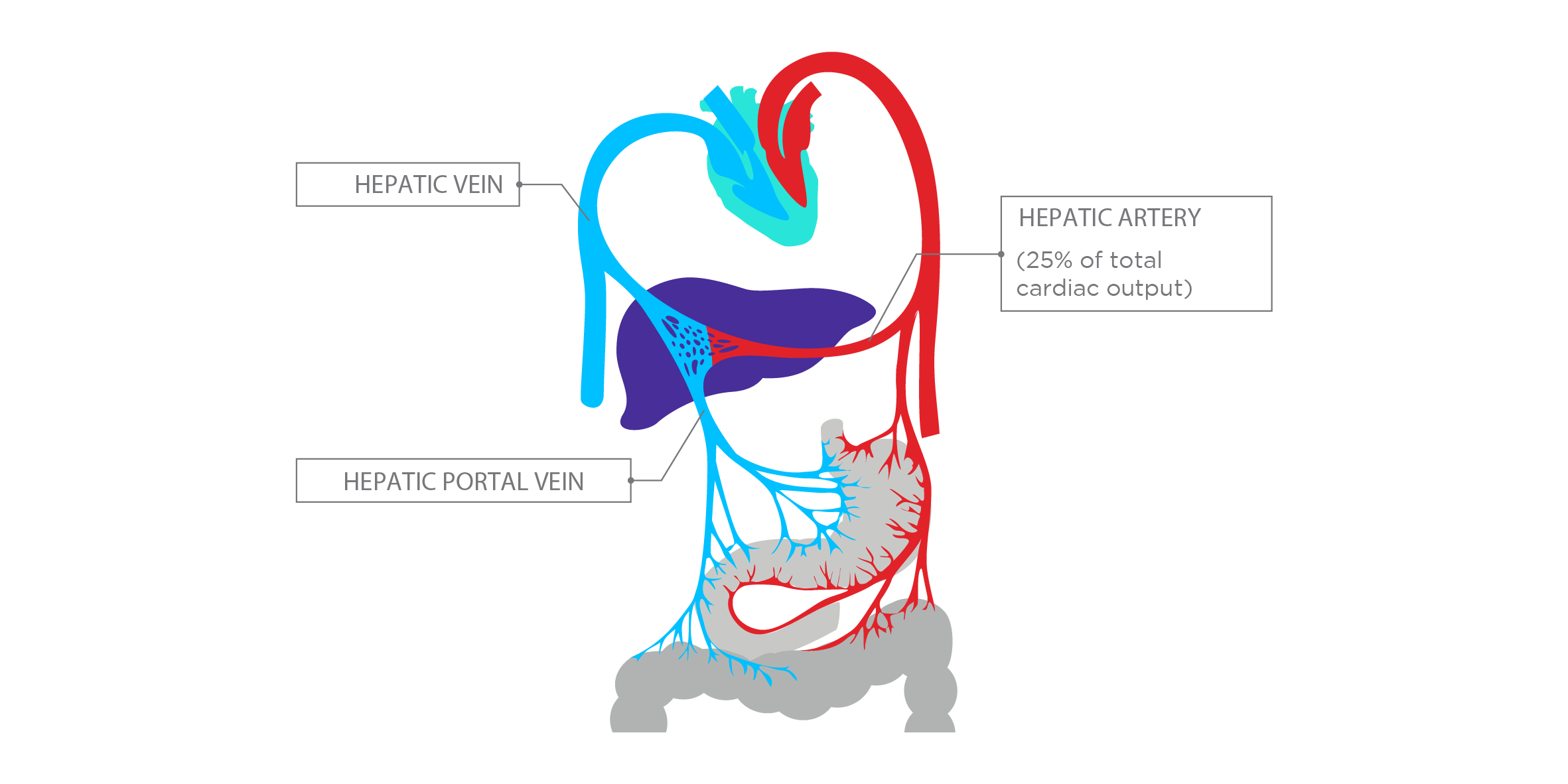
High blood supply is one of the features of the liver that makes it well suited to monitoring through breath collection. Breath analysis typically detects small-molecules known as volatile organic compounds (VOCs) that are often the end products of the body’s metabolism.The abundance of these in breath can be affected by metabolic changes associated with the progression of different illnesses. VOC metabolites end up in exhaled breath either from local lung and airway tissues, or via gas exchange with the bloodstream, which collects and carries VOCs from all over the body.
The liver receives around 25% of cardiac output but is only approximately 2.5% of total body weight [6]. The blood supply to the liver is unique, being that it receives both oxygenated and partially deoxygenated blood. The highly oxygenated blood arrives from the aorta via the hepatic artery, while the remaining 75% of the blood arriving at the liver comes from the portal vein system; carrying partially deoxygenated blood drained from the stomach, intestine, spleen, and pancreas which then reaches the liver [7]. Blood from the digestive system must flow through the liver before it reaches further destinations. This blood carries nutrients, medication and toxic substances, which need to be processed, stored, altered, detoxified, and passed back into the blood or released in the bowel to be eliminated.The rich blood supply through the liver combined with its high metabolic activity means that it is a primary source of VOCs in exhaled breath.
The liver is a key site for protein synthesis and metabolism. Research [8] has linked the production of endogenous VOCs to various metabolic processes [9], indicating the liver as an abundant source of VOCs [10]. For example, since the liver plays a vital and complex role in various metabolic and synthetic functions, damage to its cells results in an increased concentration of toxic metabolites in systemic circulation. Further research is needed to fully understand the metabolic pathways from which VOCs arise and how these can be exploited clinically using breath collection [11].
As highlighted in our previous blog, specific patterns of breath biomarkers have been associated with various liver diseases, particularly cirrhosis [12]. With proper validation and development, these VOCs could be used for diagnosis, progression monitoring and to identify treatment options. Key applications could include detecting and staging hepatic encephalopathy and predicting steatohepatitis in patients with nonalcoholic fatty liver disease.
Longer term, biomarkers could assist with the monitoring of patients who have been prescribed treatment and for those with asymptomatic early-stage liver disease to monitor progression and the effects of lifestyle changes before embarking on treatment options. Exogenous VOC (EVOC®) Probes have been developed by Owlstone Medical to enable targeted stimulation of metabolic pathways. EVOC Probes can be incorporated into new and existing liver disease studies, especially where naturally occurring VOCs are not sufficient.
At present, liver disease diagnosis is mainly conducted through invasive procedures, which are costly, and impact patient health and wellbeing. A tissue biopsy, alongside a liquid sample, is only able to assess one site or function of the liver at a specific time. With Breath Biopsy® we can analyse VOCs from throughout the body with the potential to provide a more comprehensive view of a patient’s health and potential areas for further examination. Breath Biopsy is non-invasive and enables longer-term monitoring of the patient through repeated testing in a manner that is currently impossible for people with, or suspected of having liver disease. Find out more about why Breath Biopsy is an effective approach for sampling VOCs from around the body.
References
- https://files.digital.nhs.uk/79/2031FC/nhs-out-fram-ind-feb-19-comm.pdf
- https://www.britishlivertrust.org.uk/
- http://centerforda.com/
- Petta et al. (2019). Non-alcoholic fatty liver disease/Non-alcoholic steatohepatitis patients with advanced liver disease had high burden of comorbidities, healthcare resource utilization and costs: Results from Italian administrative databases. J. Hepatology., DOI: 10.1016/S0618-8278(19)30067-2
- Newsome et al. (2018). Guidelines on the management of abnormal liver blood tests. J. Gastroenterology and Hepatology., DOI: 10.1136/gutjnl-2017-314924
- Hepatic Circulation: Physiology and Pathophysiology. Lautt, W. 2009. CA, USA: Morgan & Claypool Life Sciences.
- http://www.hepctrust.org.uk/information/liver/how-liver-works
- Lang et al. (2018). Interaction of volatile organic compounds and underlying liver disease: a new paradigm for risk. Biol Chem. DOI: 10.1515/hsz-2017-0324
- https://www.owlstonemedical.com/science-technology/voc-biomarkers/
- Khalid et al. (2014). The Liver Breath! Breath Volatile Organic Compounds for the Diagnosis of Liver Disease. Clinical Gastroenterology and Hepatology. DOI: 10.1016/j.cgh.2013.10.032
- https://www.owlstonemedical.com/about/blog/2019/may/14/why-should-we-care-about-biology-behind-exhaled-vo/
- Dadamio et al. (2012). Breath biomarkers of liver cirrhosis. J. Chromatography B. DOI: 10.1016/j.jchromb.2012.07.025