Breath-based VOCs in current gastrointestinal research
Published on: 23 Aug 2021

Owlstone Medical recently began collaborating with Functional Gut Diagnostics and Functional Gut Clinic to discover, validate and commercialize new breath tests for digestive health disorders. In her first guest blog, Sarah Bloor, Clinical GI Physiologist at Functional Gut Diagnostics, shared her perspectives on the current usage of breath testing in the gastrointestinal field. This second blog takes a closer look at some of the ongoing research efforts to identify new breath-based biomarkers for use in gastrointestinal health.
Breath testing in Gastrointestinal health
Volatile organic compounds (VOCs) are biomarkers of human metabolic processes and can indicate clinical and nutritional status of individuals. There are over 1,000 volatile organic compounds (VOCs) that have been detected in breath. These consist of endogenous VOCs from physiological and pathological mechanisms in the body, along with exogenous VOCs which are based upon an individual’s diet, medication and their microbiome.
Research looking into the role of VOCs on gut health for the diagnostics, disease monitoring and personalised treatments has until recently been minimal. Using VOCs in digestive health could allow us to develop an understanding of the VOC signatures produced by different species in the microbiota and the VOCs which the body itself produces that indicate responses to microbiome metabolism. This knowledge could be applied via breath tests to help phenotype diseases, predict optimal treatment outcomes and better understand how treatments actually work.
Investigating the impact of iron on the gastrointestinal tract
The Functional Gut Clinic, Functional Gut Diagnostics and Owlstone Medical are working together to discover, validate and commercialise novel tests that link VOCs detectable on breath to digestive health disorders. Our first joint study is investigating the impact of iron on the gastrointestinal tract.
Iron deficiency affects up to 25% of the worldwide population1, with either intravenous (IV) or oral iron therapy often prescribed to help restore iron levels. However, an important unexplained clinical limitation of oral iron therapy is that it often causes significant gastrointestinal side effects such as constipation, abdominal pain and bloating, whereas IV therapy does not2.
This clinical study aims to investigate whether methane is the cause of oral iron induced constipation3. Methane is produced by methanogenic species, called archaea, which have been associated with slowing of oro-caecal and whole gut transit time and non-propagating contractions of the intestines4, 5, 6.
One metabolic pathway of particular interest to this project is the archaeal mevalonate pathway. This pathway is important for the formation of isoprenoids for the archaeal cell wall. The lipids present in archaeal cell walls are vital in differentiating between archaea and bacteria7. As the mevalonate pathway is used by archaea, and not by bacteria, measuring changes in isoprene and other isoprenoids in breath could be a way of measuring methanogenic growth in the human gastrointestinal tract.
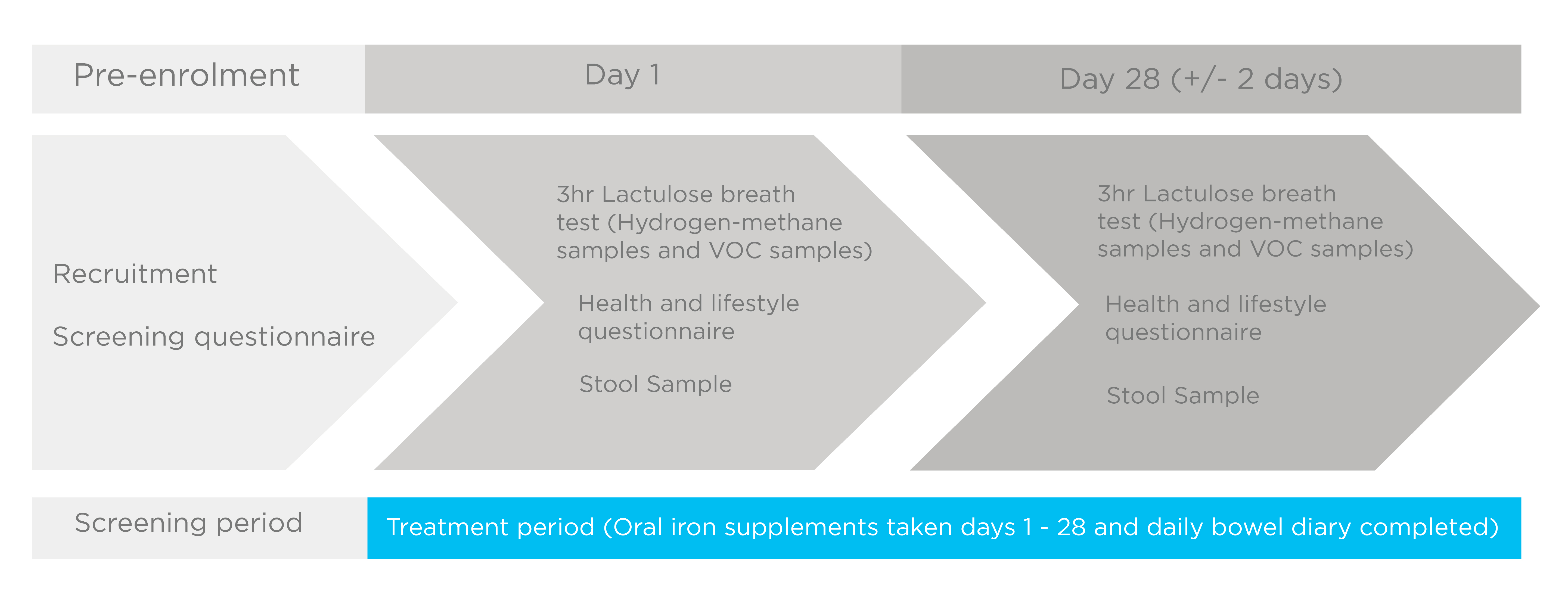
This project utilises Functional Gut’s current method of hydrogen and methane-based breath testing (HMBT) alongside Owlstone Medical’s Breath Biopsy® technology to collect and analyse VOC breath samples in healthy volunteers. Baseline breath samples are collected, and participants are then given a carbohydrate probe known to provoke intestinal fermentation, before taking subsequent breath samples. This will allow the identification of microbiota associated VOCs and the distinct VOC profile of the small bowel and colon in healthy volunteers and as a result of oral iron supplementation. This project will be supplemented with stool sample analysis to begin to associate VOCs with different species of the microbiota. These breath tests are then repeated after 28 days (+/- 2 days) of 200mg ferrous sulphate (65mg elemental iron) taken twice daily.
Outcomes of the project may allow us to see changes in the fermentation profile of the gut microbiota in response to oral iron and help us to investigate why oral iron supplements trigger gastrointestinal side effects. It may also be possible to see if the presence of any potential breath biomarkers can predict the poor tolerability of oral iron. Finally, it’s an opportunity to increase our understanding the wealth of VOCs produced by the microbiota and begin to differentiate the VOC profiles of the small intestine and the colon.
More information on this study
Benefits of working with VOCs in breath
VOCs can be sampled in a number of different ways including from breath, faeces, saliva and urine8. Breath testing is non-invasive, and unlike other sampling methods, patients can produce an almost unlimited amount of exhaled breath, making it an excellent and reproducible sampling source. Breath sampling has the capability to capture the production of many different compounds from different physiological and pathological processes within the body. The use of a carbohydrate probe can allow for the depiction of VOCs from the microbiome versus the hosts metabolism.
VOC research in GI disorders
Gastro-oesophageal reflux
Hydrogen and methane-based breath testing has found a high prevalence of intestinal dysbiosis in individuals with reflux9. Further research with VOC analysis has found that short chain fatty acids (SCFAs) as a result of colonic fermentation have implications on gastric tone, which in turn triggers gastric relaxation and increase air volume in the stomach10. Colonic fermentation, when provoked by fructooligosaccharides, also increases the number of transient lower oesophageal sphincter relaxations. This has been associated with an increase in acid reflux events and reflux symptoms reported11.
Inflammatory bowel diseases (BD)
VOCs are able to distinguish between IBD patients and healthy controls with compounds such as 1-octene, 1-decene and (E)-2-nonene12 and the reduction of methane13. Breath VOC profiling is able to determine ulcerative colitis from Crohn’s disease14 and propan-1-ol and phenol have been implicated for monitoring IBD treatment15. In addition to breath VOCs, faecal VOCs have the potential to be a good non-invasive technique for the diagnosis of IBD.
Irritable bowel syndrome (IBS)
Breath sampling for VOCs has resulted in the development of 16 breath biomarkers for IBS which correlate with GI symptoms with good sensitivity and specificity. These are mostly saturated and unsaturated hydrocarbons that are also identified to be markers of oxidative stress16.
VOCs have been inferred for predicting treatment outcome in gastrointestinal diseases including IBS17. A randomised controlled trial to assess the use of probiotics and the low fodmap diet in the management of IBS found a clear faecal VOC profile pattern in those that responded vs didn’t respond to probiotics or the low FODMAP diet, with 15 and 10 compounds at baseline predicting response to the low FODMAP diet and probiotics respectively. This could suggest that VOCs can be used to predict IBS associated dysbiosis and success and failed treatment with the low FODMAP diet or probiotics along with understanding of mechanisms for therapeutic responses18.
Find out more about breath testing for gastrointestinal health
We’ve collated all our resoures related to using breath testing for gastrointestinal health on one page and our webinar with Dr Anthony Hobson unpacks further how Breath Biopsy is set to transform digestive health testing.
VISit Our gastrointestinal DISEASe hub wAtch the webinar
References
- Bethell et al. (2004) Recombinant human lactoferrin treatment for global health issues: iron deficiency and acute diarrhea J. Biometals, 17(3): 337–42. DOI: 10.1023/b:biom.0000027714.56331.b8
- Tolkien et al. (2015) Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and meta-analysis PloS one, 10(2): e0117383. DOI: 10.1371/journal.pone.0117383
- Bloor et al. (2021) Oral Iron Supplementation—Gastrointestinal Side Effects and the Impact on the Gut Microbiota Microbiology Research, 12(2): 491–502. DOI: 10.3390/microbiolres12020033
- Suri et al. (2017) Elevated Methane Levels in Small Intestinal Bacterial Overgrowth Suggests Delayed Small Bowel and Colonic Transit Gastroenterology, 152(5): S525. DOI: 10.1097/md.0000000000010554
- Pimentel et al. (2006) Methane, a gas produced by enteric bacteria, slows intestinal transit and augments small intestinal contractile activity Am J Physiol Gastrointest Liver Physiol, 290(6): G1089–95. DOI: 10.1152/ajpgi.00574.2004
- Triantafyllou et al. (2014) Methanogens, methane and gastrointestinal motility Journal of neurogastroenterology and motility, 2014 20(1): 31–40. DOI: 10.5056/jnm.2014.20.1.31
- Jain S et al. (2014) Biosynthesis of archaeal membrane ether lipids Front Microbiol, Nov 26;5: 641. DOI: 10.3389/fmicb.2014.00641
- Rondanelli et al. (2019) Volatile Organic Compounds as Biomarkers of Gastrointestinal Diseases and Nutritional Status J Anal Methods Chem, 2019: 7247802. DOI: 10.1155/2019/7247802
- Haworth et al. (2021) The prevalence of intestinal dysbiosis in patients referred for antireflux surgery Surg Endosc. DOI: 10.1007/s00464-020-08229-5
- Ropert et al. (1996) Colonic fermentation and proximal gastric tone in humans Gastroenterology, 111(2): 289–96. DOI: 10.1053/gast.1996.v111.pm8690193
- Piche et al. (2003) Colonic fermentation influences lower esophageal sphincter function in gastroesophageal reflux disease Gastroenterology, 124(4): 894-902. DOI: 10.1053/gast.2003.50159
- Arasaradnam et al. (2016) Non-invasive exhaled volatile organic biomarker analysis to detect inflammatory bowel disease (IBD) Digestive and Liver Disease, 48(2): 148–53. DOI: 10.1016/j.dld.2015.10.013
- Arasaradnam et al. Colonic fermentation – More than meets the nose Medical Hypotheses,73(5): 753–6. DOI: 10.1016/j.mehy.2009.04.027
- Hicks et al. (2015) Analysis of Exhaled Breath Volatile Organic Compounds in Inflammatory Bowel Disease: A Pilot Study J Crohns Colitis, 9(9): 731–7. DOI: 10.1093/ecco-jcc/jjv102
- Belnour et al. (2021) P85 Faecal volatile organic compounds in paediatric inflammatory bowel disease Gut, 70: A84-A85. DOI: 10.1136/gutjnl-2020-bsgcampus.160
- Baranska et al. (2016) Volatile organic compounds in breath as markers for irritable bowel syndrome: a metabolomic approach Alimentary Pharmacology & Therapeutics, 44(1): 45–56. DOI: 10.1111/apt.13654
- Van Malderen et al. (2020) Volatomics in inflammatory bowel disease and irritable bowel syndrome EBioMedicine, 54: 102725. DOI: 10.1016/j.ebiom.2020.102725
- Rossi et al. (2017) Volatile Organic Compounds in Feces Associate With Response to Dietary Intervention in Patients With Irritable Bowel Syndrome Clinical Gastroenterology and Hepatology, 1;16(3): 385-391.e1. DOI: 10.1016/j.cgh.2017.09.055