Short chain fatty acids in diseases of the gut, brain, and cancer
Published on: 13 May 2022
As many as 1,000 different volatile organic compounds (VOCs) have been found on human exhaled breath but in the ongoing search for biomarkers of both diseased and healthy metabolic pathways not all of these VOCs will be of equal utility. One particular group of VOCs that hold exciting potential are short chain fatty acids (SCFAs).
We know that SCFAs are produced in the gut as part of normal fermentation of carbohydrates, but recent studies have suggested they could provide us with key insights into both healthy and diseased metabolism all around the body.
More Gastrointestinal Disease Resources
Introducing SCFAs
Instances of metabolic disease, such as diabetes, and gastrointestinal disease, such as inflammatory bowel diseases, have seen huge growth rates across the 20th and 21st centuries across the world. As many as a billion people are estimated as being affected by various gastrointestinal diseases, while more than half a billion are estimated to have diabetes alone [1,2]. In recent years a huge amount of research has been undertaken to enable more effective diagnosis, treatment and intervention.
Increasing evidence suggests that the gut microbiota has a huge role to play in establishing and maintaining good health. Our body, on its own, is incapable of digesting much of the fibrous material we consume as part of a normal diet – we don’t naturally produce the appropriate enzymes to break these fibers down. Instead, these non-digestible carbohydrate fibers are, within a healthy body, fermented in our large intestine by our gut microbiota. The gut microbiota often interacts with the host through metabolites – small molecules that are produced by microbial metabolic processes [3].
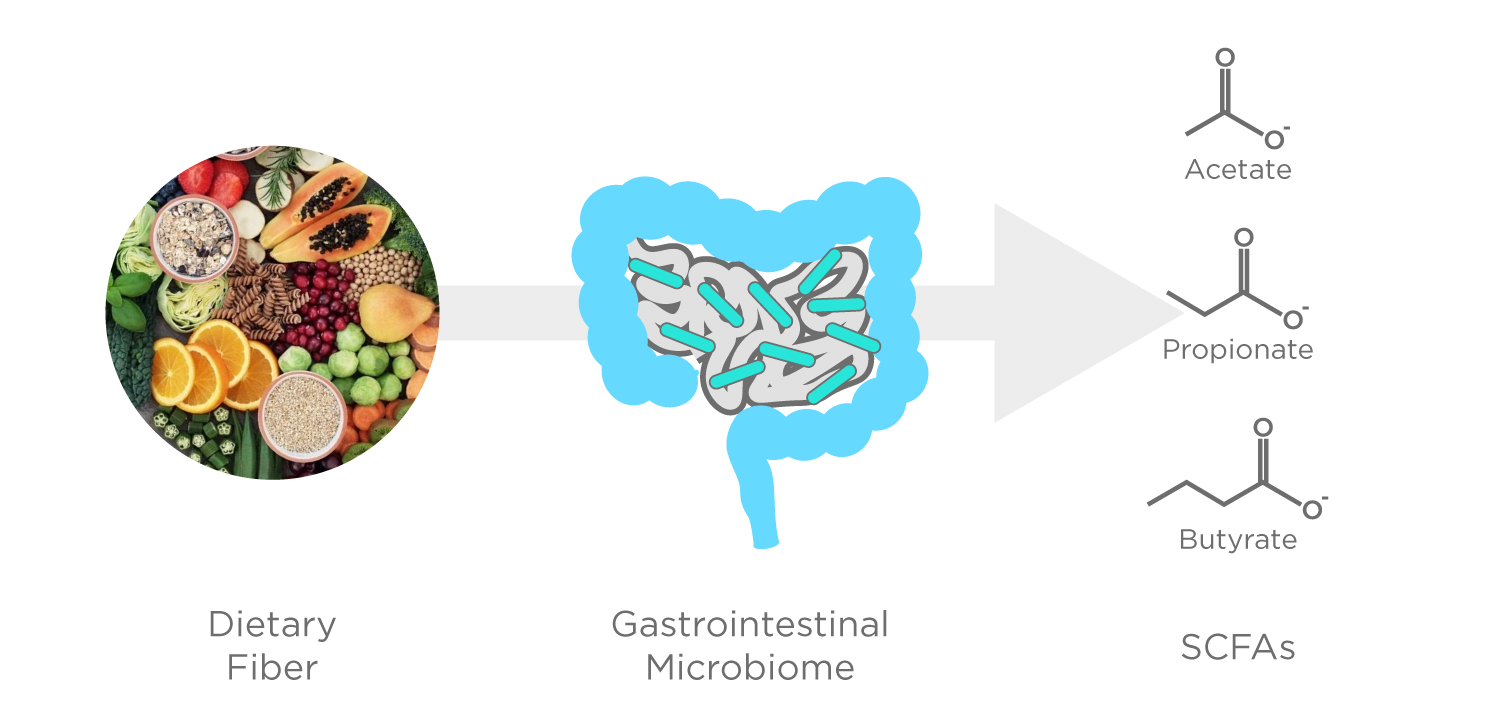
Figure 1: The microbiome releases SCFAs as a product of fermentation of dietary fiber. Adapted from Lee et al. [4]
One group of metabolites that is highly abundant in the gastrointestinal tract is short-chain fatty acids (SCFAs), saturated carboxylic acids with aliphatic tails of between 1 and 6 carbons. Three SCFAs in particular, acetate, propionate, and butyrate, make up 90-95% of the SCFAs produced in the colon [4]. Currently little is known about the exact mechanisms by which these metabolites are used within the body but studies have found the presence of all three to be linked to beneficial physiological functions in the gut and beyond.
SCFAs are volatile organic compounds (VOCs) and so can be collected, detected, and measured on human exhaled breath and from the headspace of fecal and urinary samples [4]. Many SCFAs are included in our database of the normal composition of human breath, the VOC Atlas, including acetate, butyrate, and propionate. VOCs are defined as carbon-based compounds that are gaseous at room temperature due to their chemical properties (such as high vapor pressure, and low boiling point), and like the SCFAs, can originate from inside the body to be detected in exhaled breath. In contrast to urine and feces, fasting before providing a breath sample would allow a baseline breath measurement to be taken. This could then be compared against SCFAs prominence in a patient’s exhaled breath, after more normal digestive activity. Moreover, if these SCFAs signal could be amplified by ingesting a labeled carbohydrate ‘probe’ that is metabolized by bacteria using SCFA-producing pathways, then clearer SCFA-associated signals could be collected from the breath. At Owlstone Medical we’ve already employed a similar Exogenous VOC (EVOC®) Probe approach with some success in the area of liver disease.
Watch our webinar with Anthony Hobson from Functional Gut Diagnostics on the potential of SCFAs and other VOCs as non-invasive biomarkers of gastrointestinal disease:
The many potential applications of SCFAs
As VOCs are produced through fermentation in the lower gut, it makes sense to investigate whether SCFAs have potential as biomarkers of gut function – and numerous studies have done just that. In a review paper from Parada Venegas et al., published in 2019, they examined the existing literature around the role of SCFAs in gastrointestinal wellness, finding them to be important for ‘maintaining intestinal homeostasis’ [5]. Several studies found that SCFAs have an anti-inflammatory function within the gut, reflected in the fact that reduced concentrations of SCFAs correlated with IBD diagnosis and a weakening of the epithelial gut barrier. Other studies have also linked a lack of SCFAs to Gastroesophageal reflux disease (GORD) and small intestinal bacterial overgrowth syndrome (SIBO).
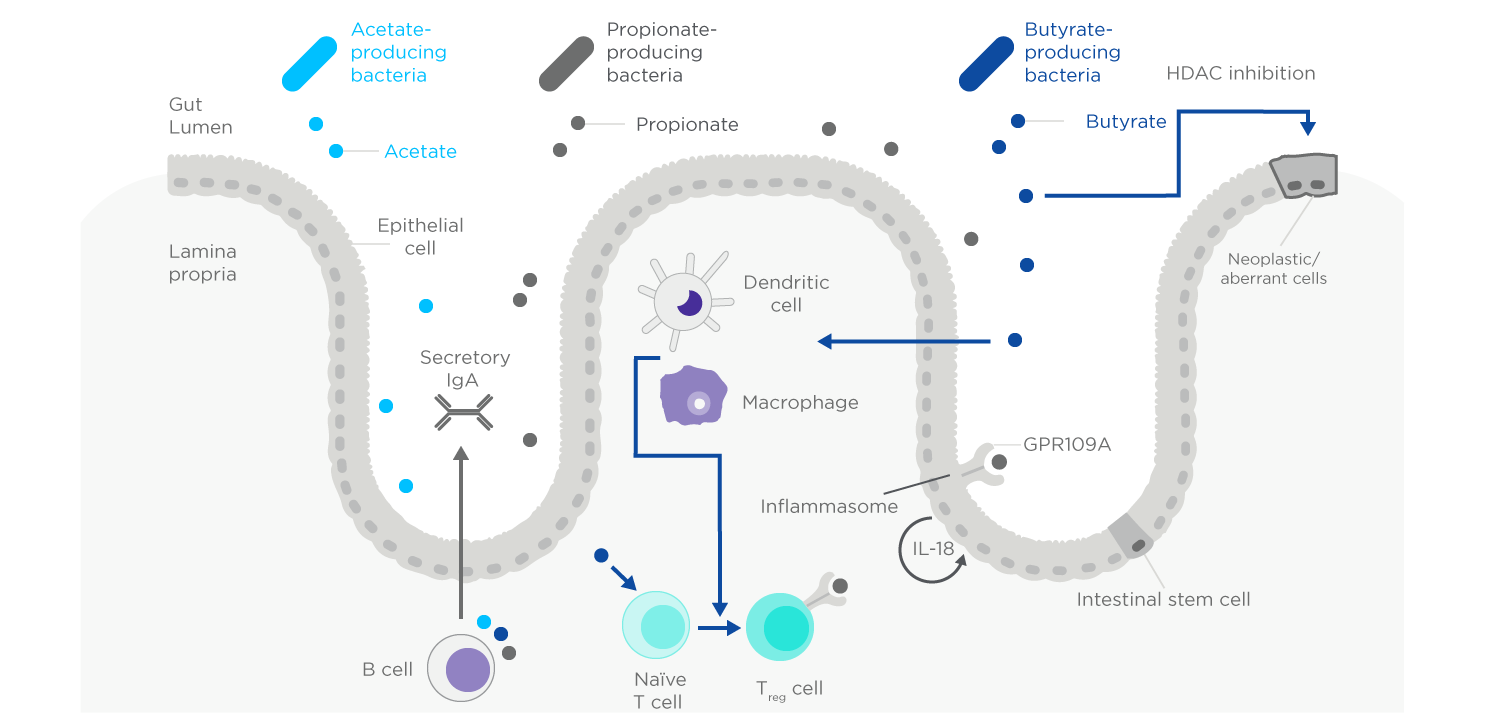
Figure 2: Examples of the complex interactions between SCFAs and aspects of the immune system. Adapted from Lavelle et al. [3]
More surprising than the roles of SCFAs in gut metabolism have been recent papers, reviewed by Silva et al. that have investigated the influence of SCFAs on the brain [6]. Silva et al. discuss explain that while the exact mechanisms by which SCFAs produced in the gut influence brain physiology and behavior are not fully understood, SCFAs are speculated to nonetheless play a key role in neuro-immunoendocrine regulation. The ability of SCFAs to cross the blood-brain barrier has already been demonstrated in rats. While further work is needed to transfer these investigations to humans, a thorough comprehension of how these metabolites participate in these complex gut-brain interactions may aid in developing novel therapeutic targets for treating central nervous system disorders.
A study published by Adam et al. in 2019 has also linked the potential of analyzing SCFAs on breath to achieving earlier diagnosis of esophagogastric cancer [7]. Their study investigated the production of fatty acids in esophagogastric cancer through both in vivo and ex vivo methods. Levels of a number of fatty acids were found to be elevated in patients with esophagogastric cancer, to the extent that ‘VFAs were higher in all samples derived from cancer patients compared with in the controls’. A diagnostic model that employed butyric acid and pentatonic acid levels was able to differentiate groups with an area under the curve of 0.80 and a 95% confidence interval.
As SCFAs are products of the normal fermentation there is evidence to suggest that in many cases it may be possible to reverse any negative shortfall within the body through simple dietary intervention [4,5]. The efficacy of such an intervention could then also be assessed through ongoing monitoring of non-invasive breath samples. This approach if successful has the potential to improve the quality of life for many people by alleviating or even reversing established gastrointestinal disease.
As demonstrated in this blog, everything we know so far seems to suggest an important role for SCFAs in maintaining good health both in the gut and around the rest of the body, but in breath research there are no guarantees. At Owlstone Medical we’re committed to investigating the role of SCFAs, alongside our partner in gastrointestinal health Functional Gut Diagnostics, but we can’t yet know for certain if they’ll turn out to be the best biomarkers for disease or treatment monitoring. However, as compounds that we already know can be found on breath, that have an active role in gut fermentation, they’re a great place to start looking – and we’ll be doing untargeted investigation and the same time to make sure we’re not overlooking an even better option.
We currently provide tests for small intestinal bacterial overgrowth and food intolerances using hydrogen and methane biomarkers produced by the gut microbiome:
Find out more about the potential for breath tests in gastrointestinal health in our guest blogs from Sarah Bloor at Functional Gut Diagnostics.
References
- Nirwan JS, Hasan SS, Babar Z-U-D, et al. Global Prevalence and Risk Factors of Gastro-oesophageal Reflux Disease (GORD): Systematic Review with Meta-analysis. Scientific Reports. 2020 2020/04/02;10(1):5814. DOI: 10.1038/s41598-020-62795-1
- Diabetes Around the World in 2021: IDF Diabetes Atlas; [cited 26th February 2022].
- Lavelle A, Sokol H. Gut microbiota-derived metabolites as key actors in inflammatory bowel disease. Nature Reviews Gastroenterology & Hepatology. 2020 2020/04/01;17(4):223-237.
- Lee JH, Zhu J. Analyses of short-chain fatty acids and exhaled breath volatiles in dietary intervention trials for metabolic diseases. Exp Biol Med (Maywood). 2021 Apr;246(7):778-789. DOI: 10.1038/s41575-019-0258-z
- Parada Venegas D, De la Fuente MK, Landskron G, et al. Short Chain Fatty Acids (SCFAs)-Mediated Gut Epithelial and Immune Regulation and Its Relevance for Inflammatory Bowel Diseases [Review]. Frontiers in Immunology. 2019;10. DOI: 10.3389/fimmu.2019.00277
- Silva YP, Bernardi A, Frozza RL. The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication [Review]. Frontiers in Endocrinology. 2020 2020-January-31;11. DOI: 10.3389/fendo.2020.00025
- Adam ME, Fehervari M, Boshier PR, et al. Mass-Spectrometry Analysis of Mixed-Breath, Isolated-Bronchial-Breath, and Gastric-Endoluminal-Air Volatile Fatty Acids in Esophagogastric Cancer. Anal Chem. 2019 Mar 5;91(5):3740-3746. DOI: 10.1021/acs.analchem.9b00148
Catch up on the presentations from the Breath Biopsy Conference 2024
