Breathe Deep, Think Big: Exploring the Gut-Brain Axis
Published on: 27 Jun 2023
What is the gut-brain axis?
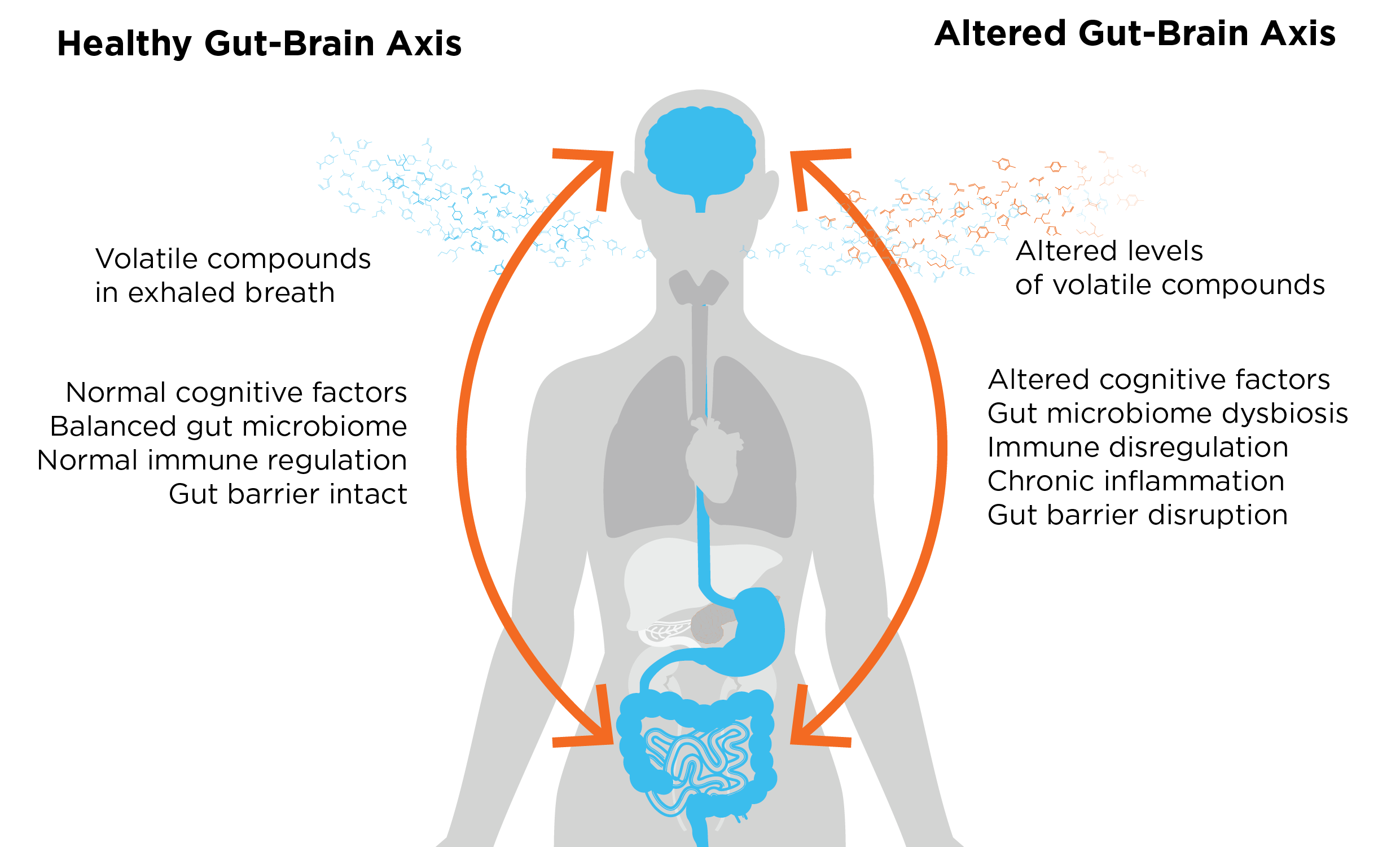
The gut-brain axis facilitates communication between the gut and the brain through a complex network of signaling molecules and pathways. Due to this intricate connection, it has the ability to influence various physiological processes, including digestion, metabolism, immune response, and mood. Clinical observations have established an association between certain gastrointestinal diseases such as irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD), and mental health conditions like anxiety and depression. This has led to the suspicion that the gut-brain axis may play a role in these common diseases that have broad, but mostly unknown mechanisms behind them.
Indeed, research has suggested the connection between the interworking of the gut-brain axis. Studies have shown physiological stress can exacerbate gut inflammation in specific bowel diseases. This process is driven by the brain, which sends out signals to release stress hormones called glucocorticoids. A recent publication by Schneider et al. has shed light on the role of glia in the gut, which are targeted by glucocorticoids and subsequently release molecules that activate immune cells, thus triggering inflammation (1).
Even more intriguingly, the gut-brain axis is further influenced by the complex interplay of microbes in the gut, giving rise to the concept of the microbiota-gut-brain axis. This dynamic relationship not only impacts the digestive system, but also the immune system and the central nervous system altogether. For example, an imbalanced microbiota, which is often associated with the disruption of the gut barrier, can activate the mucosal immune system. Consequently, molecules including inflammatory mediators and neuroactive substances are released and travel through the gut-brain axis, ultimately altering the mood and behavior.
As well as better understanding bowel conditions, the bidirectional communication of the gut-brain axis has also emerged as a crucial factor in understanding mental health disorders. Metagenomic analysis has revealed a potential association between the gut microbiome and certain mental disorders. Although the precise mechanisms underlying the influence of gut microbes on the brain are not yet fully understood, research suggests that metabolites, or metabolite derivatives (volatile organic compounds, VOCs) produced from the gut microbes are capable to distinguish between individuals with mental disorders and those that are healthy. Moreover, these VOCs can distinguish between different mental disorders. Therefore, volatile compounds produced in the gut that can be detected in exhaled breath offer an innovative new way of studying the gut-brain axis.
Breath analysis of the gut-brain axis.
One approach for assessing VOCs is Breath Biopsy®. In a study by Smolinska et al., breath VOCs and metagenomics were utilized to investigate individuals with Crohn’s Disease (CD), revealing a connection between gastrointestinal diseases, the gut microbiome, and exhaled breath (2). While there may be an influence of the microbiome and its associated gastrointestinal diseases on the brain through the microbiota-gut-brain axis potentially affecting mood, to date, the connection between gastrointestinal diseases, the gut microbiome, and its effects on the brain has not been made in exhaled breath studies. However, Henning et al. investigated utilizing breath VOCs to detect schizophrenia and depression, and connected two microbial-produced VOCs to the involvement of the microbiota–gut–brain axis (3). The study showed 5 VOCs which had a 76.8% classification accuracy to distinguish participants with major depression disorder (MDD) from healthy controls, 83.6% to distinguish participants with schizophrenia from healthy controls, and 80.9% to distinguish participants with MDD from those with schizophrenia. Of these 5 VOCs with moderate classification accuracy, two VOCs, trimethylamine and butyrate, could be further connected to the involvement of the microbiota-gut-brain axis. Both trimethylamine and butyrate are produced by the gut microbes, therefore these VOC changes suggest an association between the microbial metabolites and mental conditions. It should be noted that this study did not use blanks to distinguish between breath and background signal, and confounders like nutrition and medication need to be also taken into account. More information on how Owlstone Medical has developed a standardized method to distinguish breath VOCs from ambient air can be found here.
The most direct evidence showing a VOC crossing the blood-brain barrier is through radio labeling. A study done by Frost et al. demonstrated acetate can cross the blood-brain barrier to be taken up by the brain by labeling acetate and using PET-CT scanning (4). Like butyrate in the previously mentioned study, acetate is also a short-chain fatty acid produced by the gut microbes, thereby reinforcing the connection between the gut-brain axis. Therefore, this suggests that VOCs originating from microbes in the gut can have direct involvement in the brain as it crosses the blood-brain barrier.
We can provide all the tools and expertise you need to incorporate breath analysis into your gut-brain axis research.
As demonstrated in this blog, breath VOCs can be utilized as a tool to understand more about the gut-brain axis. There are several advantages to studying VOCs with breath. Firstly, the collection of breath samples is noninvasive and can be easily performed by individuals with different health conditions. Secondly, the diverse array of VOCs in breath can serve as potential biomarkers for various diseases and metabolic processes. Analysis of breath VOC compositions allows scientists to gain valuable insights into the physiological and pathological states of the body. Additionally, breath sampling has great potential to be performed in clinical settings or even at home.
Owlstone Medical is the world leader in breath biopsy for disease detection and precision medicine. Our recently developed VOC Atlas, a database of validated VOCs commonly present in exhaled breath of healthy individuals can be a beneficial tool to help with your research in the gut-brain axis. For example, trimethylamine, the VOC shown in Henning et al. to predict subjects with mental conditions from healthy individuals, connects the activity of the microbiota to the gut–brain axis, and can be found in our VOC Atlas. The VOC Atlas is continuously expanding and will serve as an important reference resource for the entire breath research community. If you would like more information, please contact us to discuss investigating breath VOCs for your research interest.
References
- Schneider, K.M., et al., The enteric nervous system relays psychological stress to intestinal inflammation. Cell, 2023. DOI: 10.1016/j.cell.2023.05.001
- Smolinska, A., et al., Volatile metabolites in breath strongly correlate with gut microbiome in CD patients. Anal Chim Acta, 2018. 1025: p. 1-11. DOI: 10.1016/j.aca.2018.03.046
- Henning, D., et al., Gut-brain axis volatile organic compounds derived from breath distinguish between schizophrenia and major depressive disorder. J Psychiatry Neurosci, 2023. 48(2): p. E117-E125. DOI: 10.1503/jpn.220139
- Frost, G., et al., The short-chain fatty acid acetate reduces appetite via a central homeostatic mechanism. Nat Commun, 2014. 5: p. 3611. DOI: 10.1038/ncomms4611
Catch up on the presentations from the Breath Biopsy Conference 2024
