Top 6 Breath Research Papers of 2023
Published on: 23 Apr 2024
Each year we enjoy compiling a few of our favorite breath research papers from the previous 12 months. 2023 proved to be an exciting year within breath analysis, and we have summarized a few of the pieces of research we believe helped to shape the future of the field.
Origin of breath isoprene in humans is revealed via multi-omic investigations, Sukul et al (2023), Communications Biology
Our first paper features what is considered to be one of the most abundant volatile organic compounds (VOCs) in breath, isoprene. Isoprene, or 2-methyl-1,3-butadiene, is endogenously produced in both plants and animals for the synthesis of steroid hormones and terpenoids, and its polymers are the main components of natural rubber.
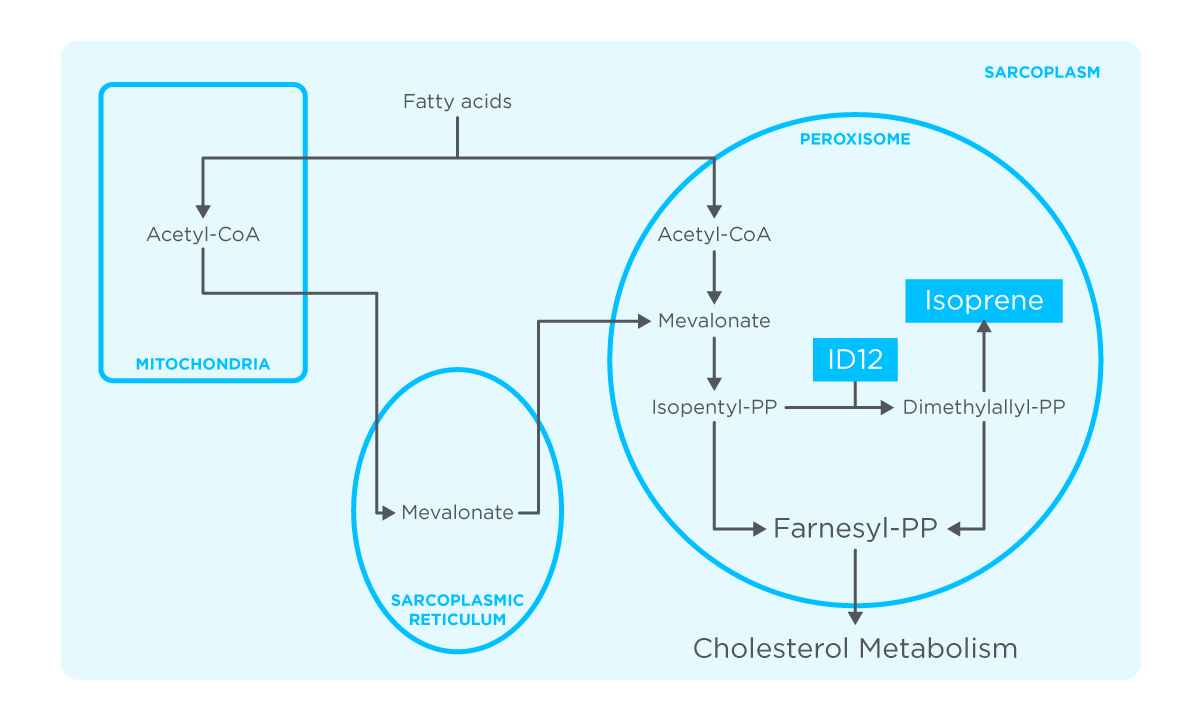
Figure 1: Metabolic pathway of isoprene production in human skeletal-myocyte. Figure based on results from study by Sukul et al. 2023.
Isoprene has been reported as a potential breath-based biomarker for a range of diseases but the unknown metabolic origin has hindered the translation of isoprene as a biomarker into clinical practice. This research paper investigated the metabolic pathways of isoprene production, using a unique and powerful approach.
Breath samples from 2000 people were taken, with isoprene levels in the exhaled breath being categorized as normal, deficient, or absent. Just five people had no isoprene in their breath and were invited back for further multi-omics investigations, including whole exome sequencing, breathomics, and serological analyses.
The results suggested that isoprene originated from muscular metabolism, and therefore measuring levels of isoprene in the breath could be of interest to musculoskeletal medicine and exercise science. This also represented an interesting approach to overcoming the key challenge of breath research: uncovering the origin of more VOCs in breath for better translatability to the clinic.
The Detection of Primary Sclerosing Cholangitis Using Volatile Metabolites in Fecal Headspace and Exhaled Breath, van Vorstenbosch et al (2023), Metabolites
Primary sclerosing cholangitis (PSC) is a chronic liver disease in which the bile ducts both in and outside the liver become inflamed, they can eventually narrow or become blocked. Diagnosing PSC can be difficult and includes invasive tests such as blood sampling, imaging, and liver biopsy.
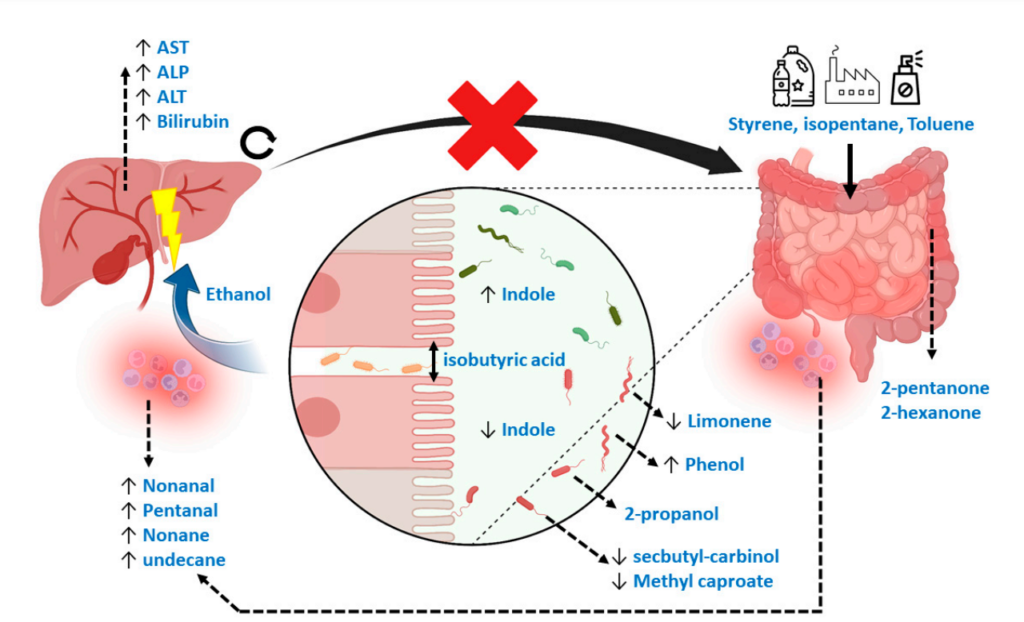
Figure 2: Mechanistic overview of the potential Volatile Metabolic markers in fecal headspace. From figure 7 in study by van Vorstenbosch et al 2023.
Patients with IBD are more likely to develop PSC and this study was aimed at identifying a method for the early detection of PSC in IBD patients via VOCs from fecal headspace and exhaled breath analysis.
Fecal material and exhaled breath were collected from 73 patients, with PSC detection resulting in areas under the ROC curve (AUCs) of 0.83 and 0.84 based on fecal headspace and exhaled breath, respectively. The results of both sampling mediums correlated to each other and to known blood biomarkers for liver disease.
Exogenous Volatile Organic Compound (EVOC®) Breath Testing Maximizes Classification Performance for Subjects with Cirrhosis and Reveals Signs of Portal Hypertension, Ferrandino et al (2023), Biomedicines
Cirrhosis detection in primary care relies on low-performing biomarkers, therefore there is potential for a non-invasive, breath test that could be implemented in primary care to increase the rates of early detection, and therefore improve prognosis and survivability.
This study compared 29 ultrasound-confirmed cirrhosis participants and 29 healthy controls to assess the performance of Owlstone’sEVOC limonene breath test in cirrhosis detection. All subjects showed a >100-fold limonene spike in breath after administration of limonene compared to the baseline sample, and the best–performing timepoint post-administration was 60 mins, with an area under the receiver operating characteristic curve (AUROC) of 0.91, sensitivity of 0.83 ± 0.07, and specificity of 0.9 ± 0.06. These results show the potential of a breath test for the early detection of liver cirrhosis within a primary care setting, and demonstrate the ability of a dynamic EVOC probe approach to increase the diagnostic performance of a breath test by increasing signal-to-noise.
Analysis of exhaled breath to identify critically ill patients with ventilator-associated pneumonia, Felton et al (2023), Anaesthesia
Ventilator-associated pneumonia (VAP) commonly occurs in critically ill patients and can extend the hospital stay by an average of 9.6 days. Diagnosis of VAP is difficult due to the limited accuracy of chest x-ray and sometimes the use of bronchoscopy or blood cultures. Due to diagnosis often relying on clinical suspicions and the limitations of the current diagnotic tests, this can result in the overuse of antibiotics, and in turn promotes antimicrobial resistance. This proof-of-concept study considers the non-invasive diagnosis of ventilator-associated pneumonia in intensive care via VOCs within exhaled breath.
Breath samples from 92 patients were analyzed and the four candidate biomarkers were benzene, cyclohexanone, pentanol, and undecanal, with an AUROC ranging from 0.67 to 0.77 and negative predictive values from 85% to 88%.
Metabolic insights at the finish line: deciphering physiological changes in ultramarathon runners through breath VOC analysis, Chou et al (2024), Journal of Breath Research
A naughty pick for our final selection as this paper was published in January 2024! We know that moderate exercise has many positive impacts on human health, but increasing the duration and intensity of exercise beyond a reasonable level into exhaustive exercise may result in negative physiological impacts on the body.
This study, conducted by the Mayo Clinic, took breath samples from 24 runners in the Ultra-Trail du Mont-Blanc ultra-marathon, which takes please over 171 kilometers and 10,000 meters of positive elevation gain, 24−72 hours before the race and 1–4 hours after the six-day event.
After analysis via GC-MS, VOCs were identified that reflect physiological changes after exhaustive exercise and were in the chemical classes of ketones, alcohols, alkenes, carboxylic acids, siloxanes, carboxylic esters, and diazoles.
This suggests that processes such as fatty acid oxidation, inflammation, and possible altered gut microbiome may be involved in the body’s response to exhaustive exercise.
If you have enjoyed this blog, do take a look at our favorite papers from 2022!
References
- Sukul P, Richter A, Junghanss C, Schubert JK, Miekisch W. Origin of breath isoprene in humans is revealed via multi-omic investigations. Commun Biol. 2023 Sep 30;6(1):1–12. doi:10.1038/s42003-023-05384-y
- van Vorstenbosch R, van Munster K, Pachen D, Mommers A, Stavropoulos G, van Schooten FJ, et al. The Detection of Primary Sclerosing Cholangitis Using Volatile Metabolites in Fecal Headspace and Exhaled Breath. Metabolites. 2023 Dec 29;14(1):23. doi:10.3390/metabo14010023
- Ferrandino G, Ricciardi F, Murgia A, Banda I, Manhota M, Ahmed Y, et al. Exogenous Volatile Organic Compound (EVOC®) Breath Testing Maximizes Classification Performance for Subjects with Cirrhosis and Reveals Signs of Portal Hypertension. Biomedicines. 2023 Nov 1;11(11):2957. doi:10.3390/biomedicines11112957
- Moura PC, Raposo M, Vassilenko V. Breath biomarkers in Non-Carcinogenic diseases. Clinica Chimica Acta. 2024 Jan 1;552:117692. doi:10.1016/j.cca.2023.117692
- Felton TW, Ahmed W, White IR, van Oort P, Rattray NJW, Docherty C, et al. Analysis of exhaled breath to identify critically ill patients with ventilator-associated pneumonia. Anaesthesia. 2023;78(6):712–21. doi:10.1111/anae.15999
- Chou H, Arthur K, Shaw E, Schaber C, Boyle B, Allsworth M, et al. Metabolic insights at the finish line: deciphering physiological changes in ultramarathon runners through breath VOC analysis. J Breath Res. 2024 Feb;18(2):026008. doi:10.1088/1752-7163/ad23fa