Explore Tuberculosis Through the Power of Breath Analysis.
Published on: 15 Jan 2024
Tuberculosis (TB) is a major global health threat, with one in four people across the globe known to be infected with Mycobacterium Tuberculosis (M. Tuberculosis). Between 5-15% of infected individuals are likely to develop active TB during their lifetime (1). TB accounts for about 10 million cases and 1.5 million deaths every year with low socioeconomic groups carrying the largest burden of TB (2). This means that despite being preventable and curable, TB is the world’s top infectious killer.
As mentioned previously, about a quarter of the global population is infected with TB, but most of these people will not develop TB disease and therefore cannot transmit it. People with compromised immune systems, such as people with HIV, malnutrition, or diabetes, have a higher risk of falling ill (3). TB is the leading cause of death among people living with HIV, as individuals with HIV are 18 times more likely to develop TB disease than people without HIV. They are also 3 times more likely to die during TB treatment, highlighting the need for high-quality TB screening (4).
TB is an airborne bacterial infection that can affect any part of the body, most commonly the lungs. M. Tuberculosis enters the air as a droplet through the coughing and sneezing of individuals with TB in their lungs. Transmission occurs when these droplets are inhaled and passed through the nasal cavity, the upper respiratory tract, and finally reach the alveoli of the lungs (1). TB is not infectious at this stage, but if the immune system cannot keep the bacteria under control, the disease becomes infectious.
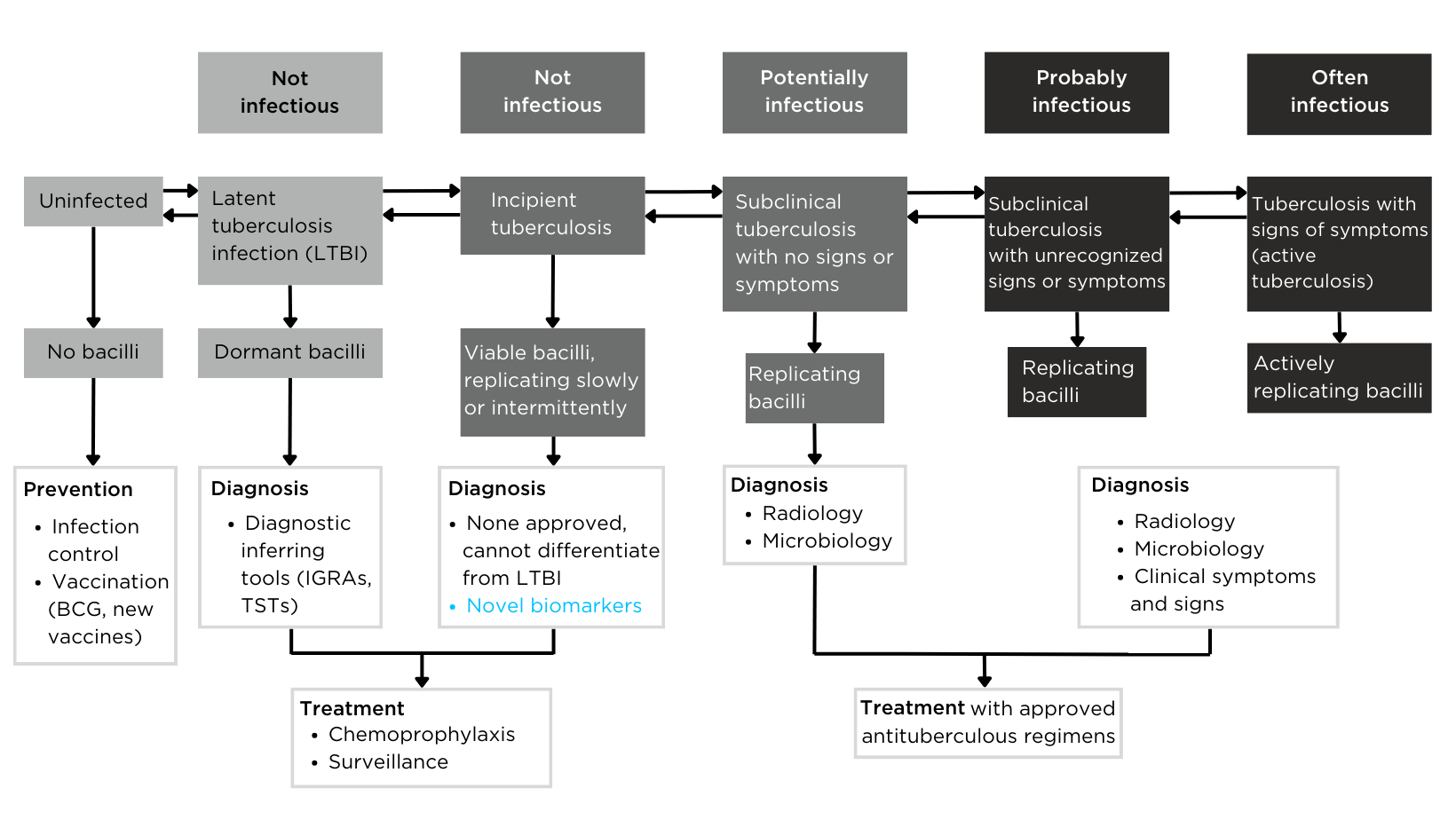
Figure 1 – The definition of tuberculosis infection based on the spectrum of tuberculosis disease.
Symptoms of TB include a cough, breathlessness, weight loss, fever, and overall weakness of the body. None of these symptoms are specific to TB, and therefore early diagnosis can be difficult (5). Testing for M. Tuberculosis is achieved either through skin or blood tests. The skin test involves an injection of tuberculin fluid into the skin of the lower arm.
Blood tests can identify if the person carries M. Tuberculosis but cannot determine if they have infectious TB, and therefore further tests including chest radiographs, CT scans, and bacteriologic examination of clinical specimens are required (1), all of which are expensive, and uncomfortable for the patient.
Therefore, the late diagnosis and invasive nature of diagnostic tests are playing a part in the mortality of this disease. A non-invasive test to help with an earlier diagnosis of TB is in desperate need to help tackle this serious disease.
Dr. Kavita Jeerage from the National Institute of Standards and Technology (NIST) recently presented at the Breath Biopsy Conference 2024, on ‘Potential Uses of Breath Surrogates for the Development and Deployment of New Infectious Disease Biomarkers’. You can watch Dr. Jeerage’s talk on-demand, as well as the rest of the talks from the conference here.
Compounds in the breath that are associated with tuberculosis.
Volatile organic compounds (VOCs) are found in various excreted biological materials and can serve as indicators of TB disease. These compounds are released into the bloodstream and reach the alveoli, where they can be excreted in exhaled breath. In TB, particularly an infection in the lungs, these VOCs can be released directly into the breath as it is in constant contact with the lungs. Therefore, VOCs found in exhaled breath are promising targets for new biomarkers for TB diagnosis and testing.
Pulmonary TB may alter VOCs in breath because Mycobacteria and oxidative stress resulting from the Mycobacterial infection generate distinctive VOCs. VOCs produced by this bacteria include C14-C26 fatty acids, as well as their methylated and hydroxylated derivatives and oxidative stress VOCs in breath include C4-C20 alkanes and methylated alkanes (6). However, as both processes are general and not specific to TB itself, further research is needed.
One study by Phillips et al found 130 different VOCs that were consistently detected in M. tuberculosis cultures in vitro, mainly derivatives of benzene, naphthalene, and alkanes (6). Another study in 2010 combined the VOCs from oxidative stress and M. tuberculosis as a biomarker for TB, with an 85% accuracy, 84% sensitivity, and 64.7% specificity (7). A study in the Philippines, UK, and India investigated a breath test with collected and concentrated VOCs from the breath of TB patients and analyzed them using gas chromatography.
This breath test only took a total of 6 minutes to carry out, and identified naphthalene, benzene, and certain alkanes as biomarkers for TB (8). This study had an 80% accuracy, which is high but still leaves room for improvement in future studies. Exogenous volatile organic compound (EVOC) probes are compounds which can be administered to patients to target TB specific mechanisms which can greatly improve the reliability of biomarker detection.
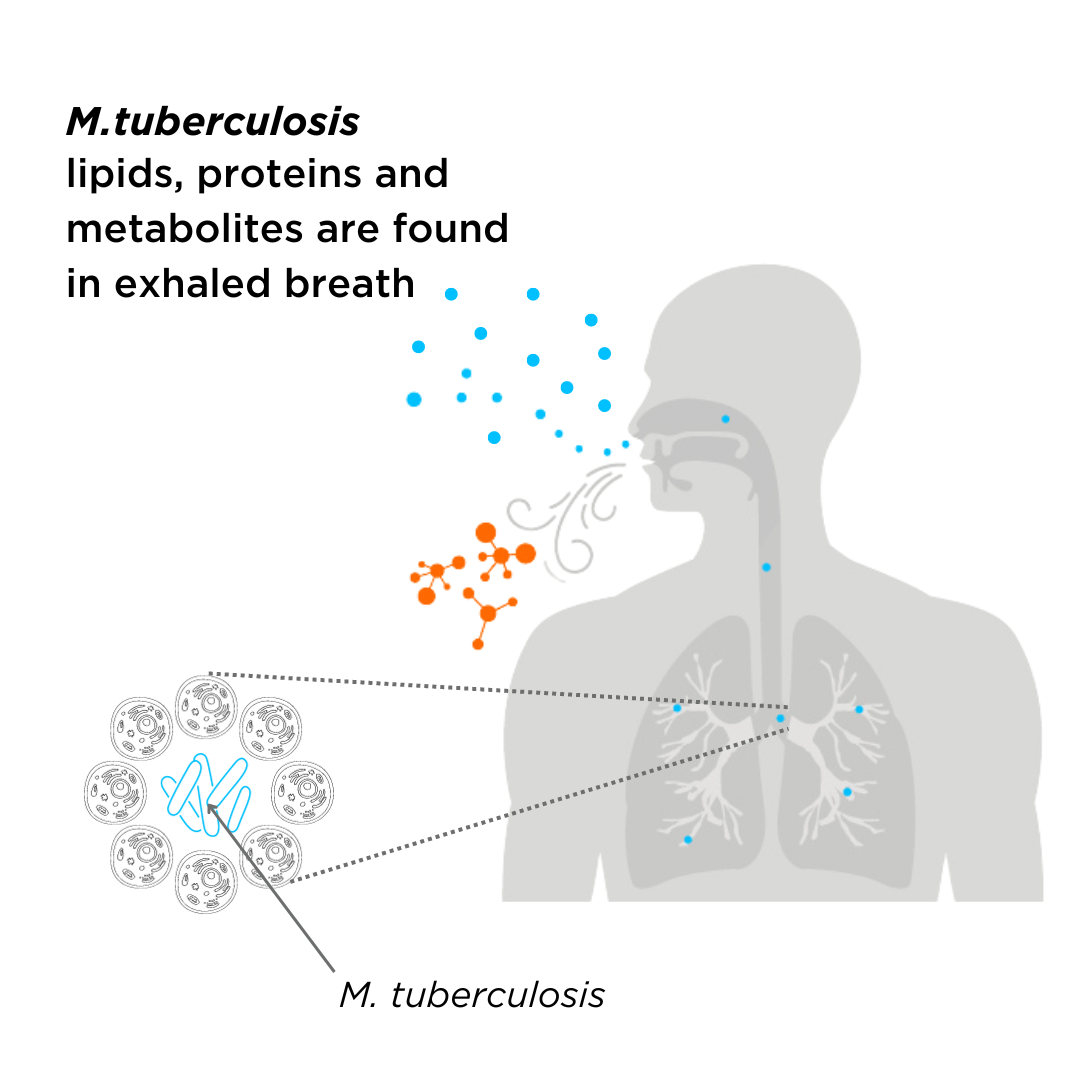
Figure 2 – VOCs originating from a tuberculosis infection are found in exhaled breath.
Breath analysis can support tuberculosis research.
VOCs that originate or are elevated from a tuberculosis infection can readily enter our lungs and be exhaled from the body in breath. These compounds can then be analyzed and provide insight into the development and pathogenesis of tuberculosis. As tuberculosis predominantly affects the lungs, and breath is a sampling medium that is in direct contact with the lungs, analysis of breath can provide a better insight into the disease as opposed to blood or urine which are more indirect.
Breath is a virtually inexhaustible resource, with large volumes able to be collected at frequent intervals, meaning breath analysis can provide an almost real-time longitudinal analysis of VOCs. The non-invasive nature of breath analysis makes it more attractive than sputum samples or blood tests which can be uncomfortable for the patient.
We are the leaders in breath research for the early detection and precision treatment of disease, both of which are vital in the diagnosis of tuberculosis. We are here to help you include breath analysis in your research. Breath Biopsy OMNI can provide everything you might need to start or continue using breath analysis, and you can receive expert advice from our team of scientists. Many of the compounds mentioned previously, such as alkanes, are included in our VOC Atlas. You can cross-check your data against our VOC Atlas to better understand the baseline levels of VOCs in a healthy population and confidently validate your tuberculosis biomarkers.
References.
- Agyeman AA, Ofori-Asenso R. TB—an overview. J Public Health Emerg [Internet]. 2017 Jan 6 [cited 2024 Jan 11];1(1). Available from: https://jphe.amegroups.org/article/view/3668
- Raviglione M, Sulis G. TB 2015: Burden, Challenges and Strategy for Control and Elimination. Infect Dis Rep. 2016 Jun;8(2):6570. DOI: 10.4081/idr.2016.6570
- Tuberculosis [Internet]. [cited 2024 Jan 11]. Available from: https://www.who.int/health-topics/tuberculosis
- Tuberculosis & HIV [Internet]. [cited 2024 Jan 11]. Available from: https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/hiv/treatment/tuberculosis-hiv
- Campbell IA, Bah-Sow O. Pulmonary TB: diagnosis and treatment. BMJ. 2006 May 18;332(7551):1194–7. DOI: 10.1136/bmj.332.7551.1194
- Phillips M, Cataneo RN, Condos R, Ring Erickson GA, Greenberg J, La Bombardi V, et al. Volatile biomarkers of pulmonary TB in the breath. Tuberculosis. 2007 Jan 1;87(1):44–52. DOI: 10.1016/j.tube.2006.03.004
- Phillips M, Basa-Dalay V, Bothamley G, Cataneo RN, Lam PK, Natividad MPR, et al. Breath biomarkers of active pulmonary TB. Tuberculosis. 2010 Mar 1;90(2):145–51. DOI: 10.1016/j.tube.2010.01.003
- Phillips M, Basa-Dalay V, Blais J, Bothamley G, Chaturvedi A, Modi KD, et al. Point-of-care breath test for biomarkers of active pulmonary TB. Tuberculosis. 2012 Jul 1;92(4):314–20. DOI: 10.1016/j.tube.2012.04.002
Quick Start Guide: Everything you need to know about how breath analysis can be used in infectious disease research