Diabetes and the association of the gut microbiome
A significant correlation exists between breath Indole and blood glucose
| Publication information: H. Fink et al. Indole as a new tentative marker in exhaled breath for non-invasive blood glucose monitoring of diabetic subjects, Journal of Breath Research. (2022) 16 026001. DOI: 10.1088/1752-7163/ac4610
Disease Area: Diabetes Application: Ongoing monitoring Sample medium: Breath Analysis approach: PTR-ToF-MS Summary:
|
Blood glucose level (BGL) monitoring is crucial for people with diabetes, as prolonged high BGL can cause systemic vascular damage, leading to various chronic diseases. The most common approach for BGL monitoring is a finger-pricking test strip, which can be uncomfortable due to multiple daily measurements. Therefore, a non-invasive device for BGL monitoring is needed to improve the daily lives of diabetic individuals.
Breath research has gained popularity in recent decades due to its non-invasive nature. However, the connection between breath odor and diseases dates back thousands of years. In the early 20th century, diabetic patients were described as having a fruity breath odor during periods of high BGL. Now identified as acetone, the volatile organic compound (VOC) responsible for the fruity breath odor is produced when insulin regulation of glucose uptake is disrupted, known as diabetic ketoacidosis (DKA). Because VOCs such as acetone are transported through the bloodstream to the lungs and exchanged into the air at the alveolar membrane, VOCs in exhaled breath can reflect biochemical changes in the body.
Research has demonstrated a correlation between BGL and breath acetone levels [1]. However, the levels of acetone in breath can be influenced by other variables, including exercise, age, sex, and the presence of other diseases. Therefore, acetone alone is not a sufficient biomarker for BGL monitoring. Although other VOCs (methyl nitrate, ethanol, xylene) have been studied for BGL monitoring, the metabolic pathways and linkage to disease pathobiology still require more understanding.
This new study by Fink et al. conducted an untargeted analysis on exhaled breath from 60 diabetic subjects with the goal of identifying potential VOCs as markers for glucose monitoring.
Methods
Sixty patients with an established diagnosis of diabetes (30 with type 1 and 30 with type 2) provided both breath and blood samples in the fasting state and after a standardized meal. Breath samples were collected every 15 minutes for one hour during the fasting state and for five hours after a standardized meal using Proton Transfer Reaction Time of Flight Mass Spectrometry (PTR-ToF-MS). BGL was tested in parallel with blood glucose monitoring test strips.
To understand the origins of some of the more interesting VOCs in this study, specifically indole, acetate, and propionate, one healthy male subject provided both breath and blood samples at 15-minute intervals after ingesting lactulose or 13C-labeled glucose. The experiment was repeated three times in the same subject.
Results
In this study, approximately 500 VOCs were detected in exhaled breath. As shown in Table 1, the authors identified seven VOCs exhibiting the best correlation with BGL, and the results were not affected by the types of diabetes. Of these seven VOCs, five were tentatively assigned and later confirmed as formaldehyde, acetone, propionate, phenol, and indole. The other two ion fragments were tentatively identified as short-chain fatty acids (SCFAs) acetate and propionate after considering the molar mass of water.
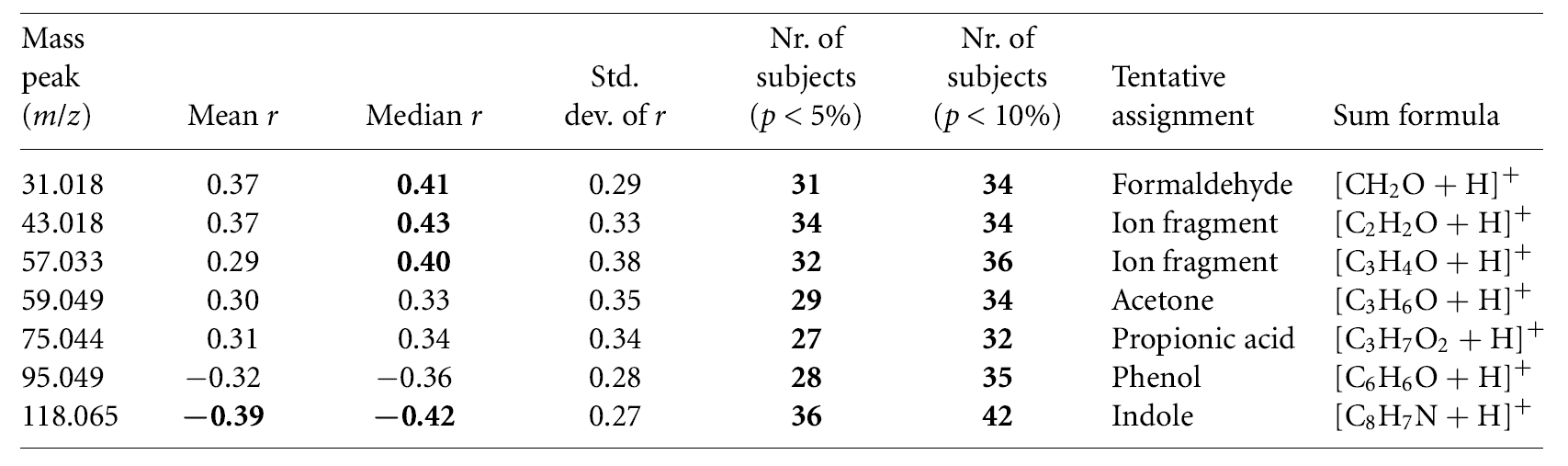
Table 1: Tentatively identified VOCs with the best correlation and a number of subjects with significant correlation to blood glucose levels (Statistically significant values are indicated in bold).
Among the seven VOCs that correlated with BGL, only indole reached a statistically significant mean correlation coefficient (p < 0.05). Indole also exhibited the highest number of subjects with statistically significant correlation (36 out of 60 subjects, p < 0.05). The mean trends of indole and glucose closely resembled each other at baseline. After the meal, levels of indole decreased while levels of BGL increased (Figure 1). Other VOCs occasionally showed levels of significant correlation with BGL in a smaller number of subjects, including those tentatively identified as SCFAs acetate and propionate (34 and 32 out of 60 subjects, respectively, p < 0.05).
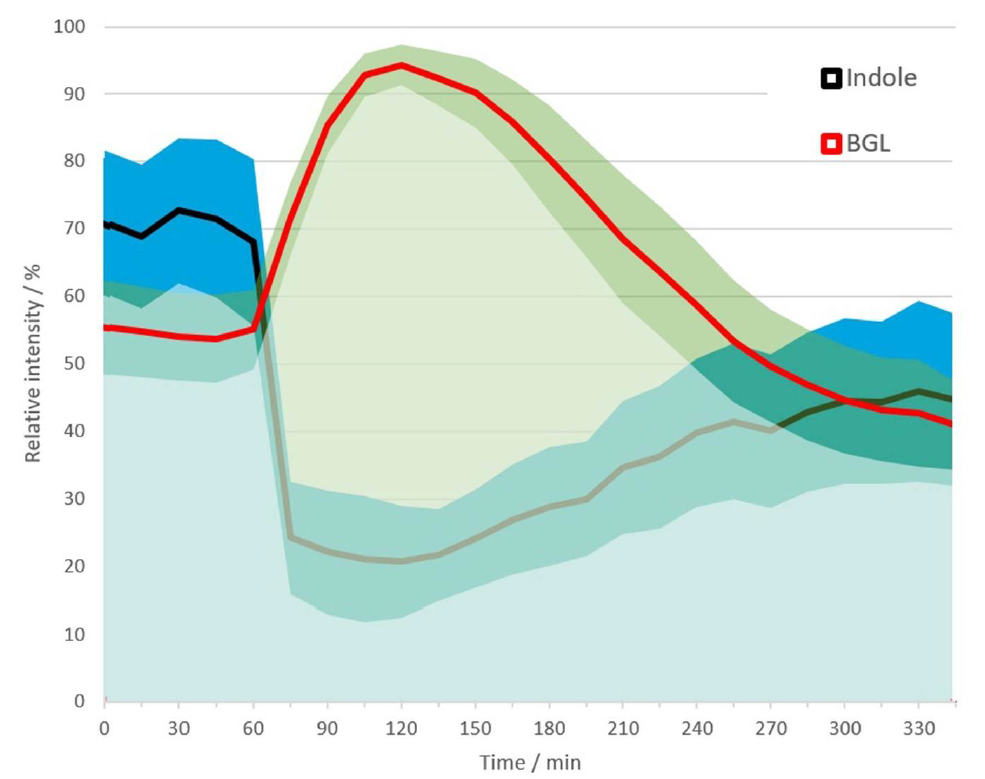
Figure 1: Mean relative trends of indole (black) and BGL (red) during measurement time across all subjects, with bands showing the standard deviation.
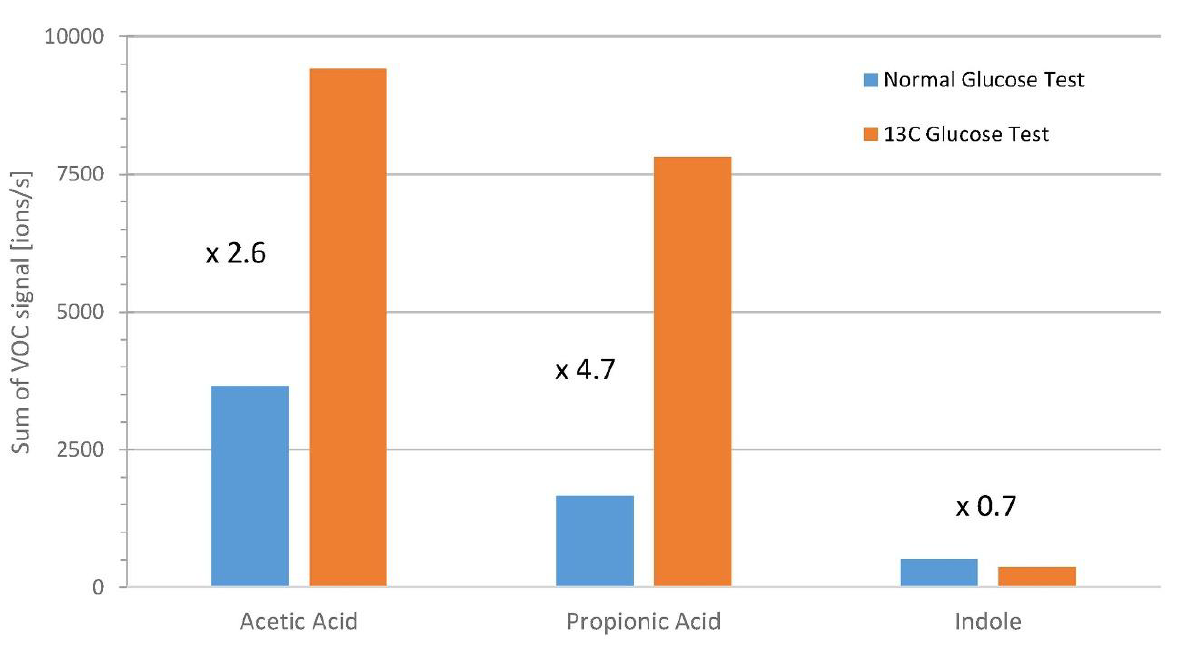
Figure 2. Cumulative signals during postprandial phases of glucose tolerance tests with normal glucose and labeled 13C glucose. Signals of 13C-VOCs were summed during phases with BGL > 140 mg/dL-1.
Discussion
This study by Fink et al. showed that exhaled breath indole, a microbial metabolite of tryptophan, is negatively correlated with BGL. It has been demonstrated that gut microbes in the Escherichia, Bacteroides, and Clostridium genera produce indole via the enzyme tryptophanase [2]. Other studies performed on rat cell lines have indicated that indole is a possible signaling molecule that stimulates glucagon-like-peptide-1 (GLP-1), a molecule required for accurate insulin response [3]. However, a prolonged increase in intracellular indole reduces GLP-1 secretion [3]. This provides a hypothesis for the decrease in extracellular indole levels (reflected in breath) and the increase in extracellular glucose levels observed in diabetic subjects by Fink et al. in this study.
The SCFAs (acetate and propionate) identified in this study are also products of bacterial metabolism. Gut bacteria metabolize carbohydrates like fibers in the large intestine, producing SCFAs. However, the positive correlation of SCFAs with BGL was short-lived during the initial time-points, and reduced in level faster than BGL. The levels of exhaled breath SCFAs also demonstrated huge variation, which could be a result of different gut microbiome compositions in subjects or the effects of medication. As the levels of SCFAs are determined by carbohydrate breakdown from bacterial glycolysis, as shown in the additional experiments using lactulose and labeled 13C-glucose, SCFAs may not be sufficient stand-alone biomarkers for BGL monitoring if diet is not controlled and the microbiome composition is unknown.
On the other hand, the levels of breath indole were unaffected by carbohydrate breakdown, as demonstrated by Fink et al. This suggests that while indole has been linked to human glucose metabolism, it is not directly affected by bacterial glycolysis. Therefore, indole has the potential to act as a biomarker for non-invasive blood glucose monitoring. However, the use of indole as a marker must be considered with caution, as similar to other microbial products, the gut microbiome composition between individuals can be a limitation of this application. A clinical study with a larger and more diverse cohort, along with metagenomics data is required to confirm the findings. Further investigation of metabolic pathways is also needed.
Owlstone Medical are interdisciplinary specialists in breath.
Our Breath Biopsy OMNI® is a platform in which we provide end-to-end optimized service for consistent breath analysis. As part of the platform, our Breath Biopsy® Collection Station ensures reliable and reproducible breath collection, with efficient and portable ambient VOC exclusion, simultaneous collection of replicate samples, and easy collection of blanks.
Recently we have developed our Breath Biopsy VOC Atlas – a catalog of more than 200 identified VOCs commonly found on breath, including gut microbiome-associated molecules like indole, several SCFAs including acetate, butyrate, and propionate, as well as aromatic amino acid breakdown products. To learn more, you can get in touch with us to discuss how we could help support your research into diseases associated with the gut microbiome.
References
- Trefz, P., et al., Non-Invasive Assessment of Metabolic Adaptation in Paediatric Patients Suffering from Type 1 Diabetes Mellitus. J Clin Med, 2019. 8(11). DOI: 10.3390/jcm8111797
- Jaglin, M., et al., Indole, a Signaling Molecule Produced by the Gut Microbiota,
Negatively Impacts Emotional Behaviors in Rats. Front Neurosci, 2018. 12: p. 216.
DOI: 10.3389/fnins.2018.00216 - Chimerel, C., et al., Bacterial metabolite indole modulates incretin secretion from intestinal enteroendocrine L cells. Cell Rep, 2014. 9(4): p. 1202-8. DOI: 10.1016/j.celrep.2014.10.032
