Stratifying acute cardiorespiratory breathlessness with breath metabolites
A robustly powered study demonstrating the utility of breath biomarkers
| Publication information: W. Ibrahim et al. Visualization of exhaled breath metabolites reveals distinct diagnostic signatures for acute cardiorespiratory breathlessness, Science Translational Medicine 2022, 14:eabl5849. DOI: 10.1126/scitranslmed.abl5849
Disease Area: Respiratory disease (asthma, chronic obstructive pulmonary disease, pneumonia and heart failure) Application: Patient Stratification Sample medium: Breath Products: ReCIVA® Breath Sampler Analysis approach: GCxGC-MS Summary:
|
More than an eighth of emergency hospital admissions in the UK are caused by breathlessness resulting from cardiorespiratory disease. However, despite patients presenting with similar symptoms, cardiorespiratory breathlessness can have a number of diverse causes (including asthma, chronic obstructive pulmonary disease [COPD], heart failure, and/or pneumonia) each of which require tailored therapeutic intervention for effective treatment. Quick and effective diagnosis is therefore key to positive patient outcomes.
Currently differential diagnoses of acute breathlessness rely on blood-based biomarkers (such as C-reactive protein and B-type natriuretic peptide) and radiology. These biomarkers perform reasonably well in patients whose breathlessness has a single cause but have limited ability to discriminate the components of multifactorial cases. Breath-based volatile organic compounds (VOCs) represent an exciting alternative, potentially allowing simultaneous analysis of diagnostic and prognostic biomarkers from both the lungs and systemic circulation.
W. Ibrahim et al. have conducted a robustly powered study that demonstrates the utility of breath biomarkers for triaging patients exhibiting acute breathlessness and show how this technology can be translated into the clinic.
Methods
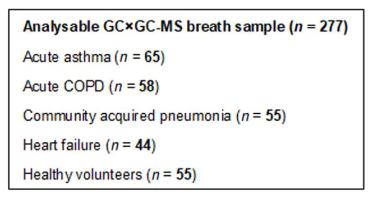
Table 1: Number of analyzable GC×GC-MS breath samples.
Breath samples were collected from 277 patients hospitalized with acute breathlessness and matched healthy controls. This included 65 patients with acute asthma, 58 with acute COPD, 44 experiencing heart failure, 55 with community acquired pneumonia and 55 healthy controls. Breath samples were collected via the ReCIVA® Breath Sampler onto adsorbent cartridges and then analyzed using TD-GCxGC-MS. Trial participants were then placed into either a discovery cohort, or a replication cohort to allow for internal replication and testing of VOC-based diagnostic models.
805 unique chromatographic features were detected across the breath samples analyzed, with an average of 404 features per sample. The data was examined and corrected for batch effects which were found to relate to instrument maintenance. No batch effects were observed on the basis of different ReCIVA units used, or other common variables.
Results
101 molecular features (MFs) were considered potential biomarkers, with 58 of these identified against standards, a further 21 MFs were assigned putative identities based on mass spectral and retention index library matches and 22 were classified based on mass spectral data.
A model based on all 101 compounds and adjusted for clinical covariates, including smoking status, time between hospital admission and breath sample collection, mEWS-2, and recent prior therapies was able to distinguish control and acute patients with an ROC-AUC = 1.0 in the replication cohort.
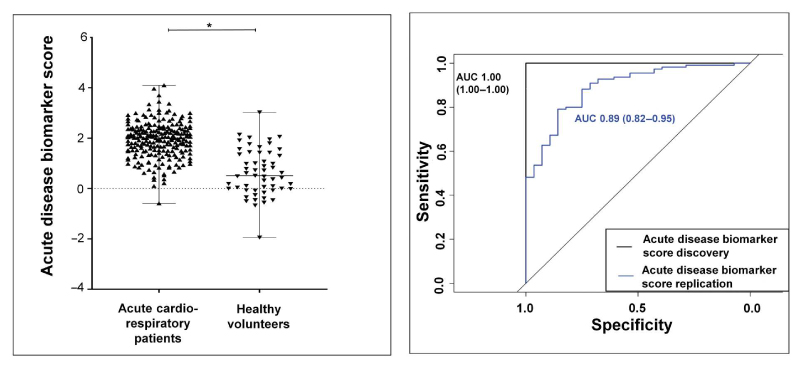
Figure 1: (Left) Scatterplot demonstrating significant difference between breath VOC biomarker score values in acute cardiorespiratory patients and healthy volunteers. (Right) ROC curve of participants in the discovery and replication cohorts.
VOC biomarker scores showed correlation with established blood biomarkers, the VOC subgroup scores for pneumonia correlated with C-reactive protein while the heart failure subgroup’s VOC biomarker scores correlated well with B-type natriuretic peptide. The VOC biomarker scores also correlated with admission observations.
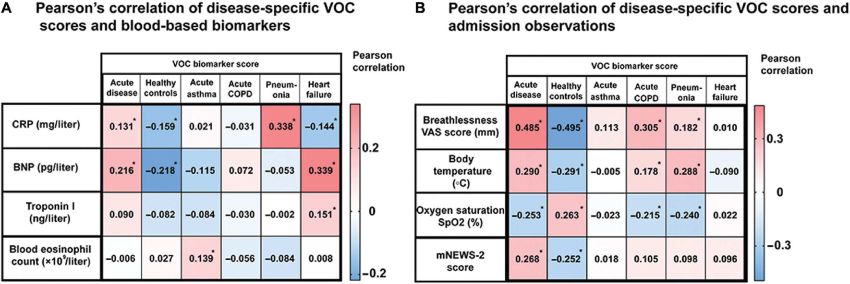
Figure 2: Correlation of VOC biomarker score with blood biomarkers and disease acuity.
Differentiating between patient subgroups using an adjusted model based on both VOC biomarker scores and possible confounding factors (as above) resulted in diagnostic accuracy as follows:
- Asthma differentiated with an AUC of 0.88
- COPD differentiated with an AUC of 0.86
- Heart failure differentiated with an AUC of 0.91
- Pneumonia differentiated with an AUC of 0.91
The modest correlations between VOC biomarker scores and individual blood biomarkers paired with the accuracy of biomarker scores in identifying disease subgroups indicate that VOCs are providing important additional diagnostic information that is not captured by blood biomarkers alone.
Discussion
The chemical classes most commonly associated with acute breathlessness hydrocarbons (30%), ketones (10%), aldehydes (8%), and terpenes (13%), followed by sulfur-containing VOCs (7%), alcohols (6%), aromatics (5%) and esters (3%). It’s not surprising that hydrocarbons and carbonyls were the most common classes, given that they are commonly asserted to the endpoints of lipid peroxidation, which would result from oxidative stress during inflammation.
While the exact biological origins of most of the 101 potential biomarkers are yet to be definitively established, multiple VOCs identified in this study have been previously associated with respiratory diseases. These include aldehydes associated with asthma such as nonanal, decanal, and hexanal; certain hydrocarbons for pneumonia and heart failure and a number of sulfur-containing VOCs for COPD.
W. Ibrahim et al. conducted a robust and well-powered study that generated a VOC-based predictive tool with the capacity to help clinicians in cases where patients have a serious but potentially non-specific symptom. However, this study relied on TD-GCxGC-MS which is a mature and reproducible technology, but one that is non-mobile and requires samples to be transported to lab facilities for analysis. Next steps in bringing VOCs to the aide of patients and clinicians will include optimization of new technologies that can be brought directly to the bedside, for the rapid triage of patients experiencing acute breathlessness.
At Owlstone Medical we’ve developed Breath Biopsy® OMNI® as an end-to-end optimized service for consistent breath analysis, and our ReCIVA Breath Sampler is just a small part of that. If you’re interested in investigating breath biomarkers for cardiorespiratory disease then, in addition to reliable breath collection and analysis methodologies, we can offer study design, management and data interpretation expertise.
If you’re looking to translate your existing findings into the clinic we can help with that too. Our FAIMS technology has the ability to rapidly monitor a broad range of VOC biomarkers with both high sensitivity and selectivity and can offer an immediate yes/no response. Get in touch to find out more.

