Advancing early detection for liver diseases with Breath Biopsy
Published on: 30 Sep 2020
One of our key priorities for Breath Biopsy® is improving the ability to detect, stage, and monitor progression or recovery from liver disease. The liver is a highly resilient organ and the signs of advancing liver disease can be missed until late stages when the damage is often severe and irreversible. Factors such as poor diet, obesity, and type-II diabetes are contributing to a rapid rise in the prevalence of liver diseases in many countries, affecting as many as 3 in 10 adults and an increasing number of children. A US study [1] found that 10% of children between the ages of 2 and 19 showed signs of non-alcoholic fatty liver disease (NAFLD).
Detecting liver diseases, such as NAFLD and non-alcoholic steatohepatitis (NASH) as well as more advanced cirrhosis, is a significant clinical challenge. Symptoms are rare and current methods of detection are often expensive and invasive involving blood or even tissue sampling. A non-invasive approach that can be offered as part of a widespread screening program for otherwise healthy individuals represents an ideal solution and we are developing Breath Biopsy to meet this need.
Our recent publication, by Ferrandino et al. [2], is our first step towards effective, non-invasive liver disease early detection. In this pilot study, we collected samples of volatile organic compounds (VOCs) with the Breath Biopsy Collection Station and performed targeted Breath Biopsy VOC analysis comparing the breath of healthy volunteers to that of patients with cirrhosis or cirrhotic hepatocellular carcinoma. Our analysis focused on limonene, a chemical that originates from food and drinks such as orange juice. We focused on limonene because the work of Professor Chris Mayhew and his team at the University of Birmingham previously identified an association with liver diseases [3]. Our work serves to validate and expand upon this previous finding using an independent approach to sample collection and analysis.
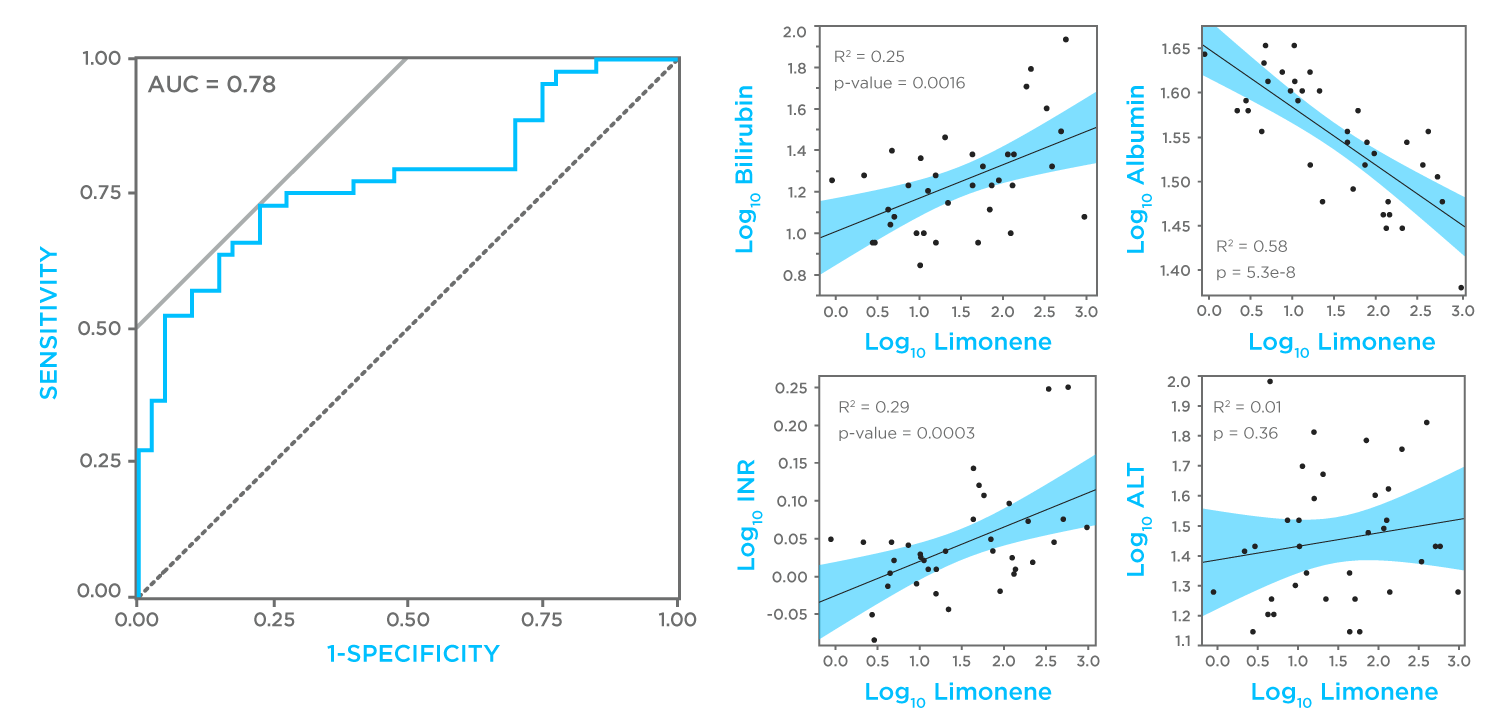
In the study, the levels of limonene in Breath Biopsy samples were higher in cirrhosis patients, especially in those with more severe disease (Child-Pugh classification). By analyzing these data we generated a model that can differentiate between healthy and cirrhotic individuals with 75% accuracy (73% sensitivity, 77% specificity). This is a small pilot study and the amount of limonene each subject consumed was not standardized, so this represents a strong result with clear means for enhancement through optimization as a probe and the addition of further markers.
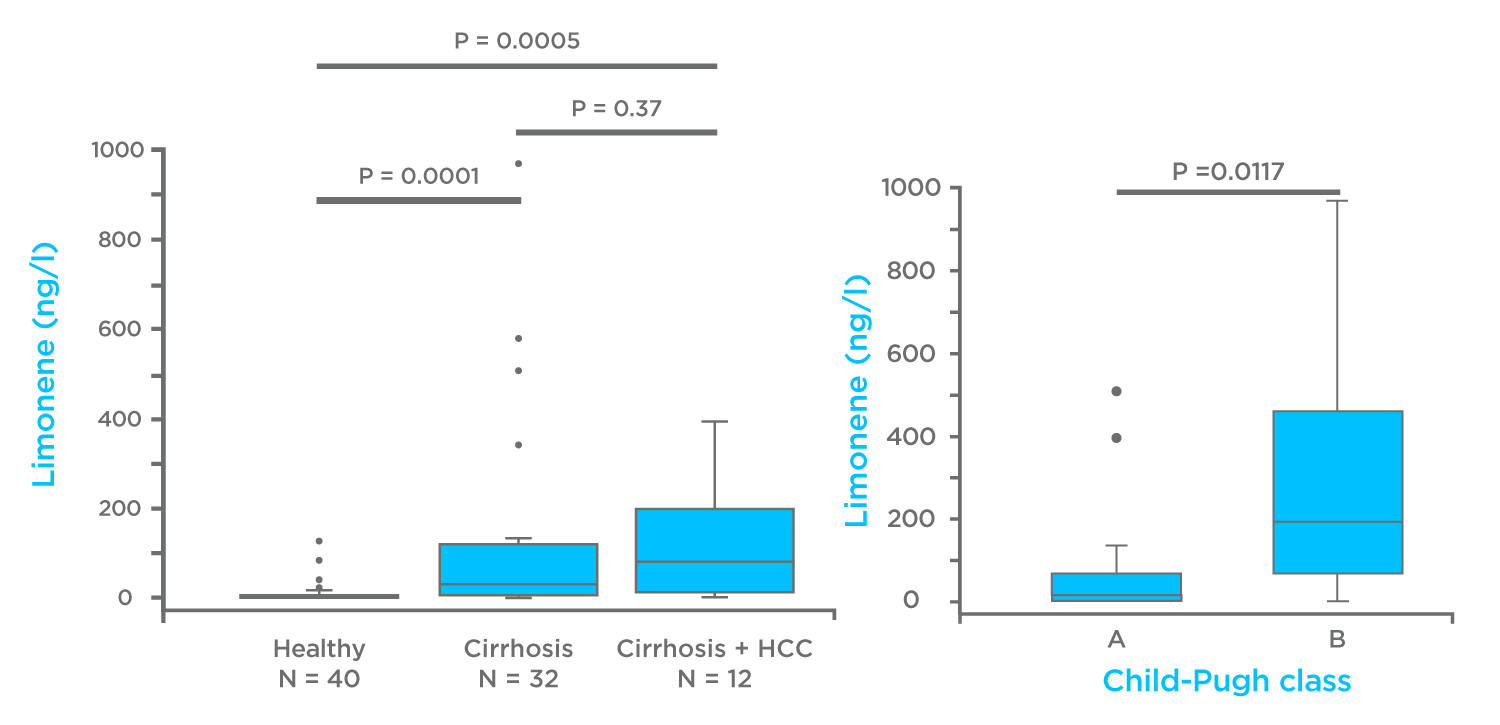
We also compared limonene measurements on breath to other known blood indicators of liver function and damage collected through more invasive approaches. We saw significant correlations with three other liver function markers (bilirubin, albumin and international normalized ratio (INR)) and no correlation with alanine amino transferase (ALT) a measure of liver damage. This indicates that limonene has great potential to detect early stage liver diseases where function may be mildly affected but liver damage is non-existent.
Limonene represents an ideal exogenous volatile organic compound probe (EVOC® Probe), a harmless VOC that originates outside the body and can be reliably and accurately detected on breath. Measuring an EVOC Probe using Breath Biopsy provides strong, clear results because the EVOC Probe dose can be standardized across test subjects and isn’t influenced or masked by other background signals within the breath. Our analysis methods can also be optimized with the EVOC Probe to ensure accurate, high-sensitivity detection. The strengths of the EVOC Probe approach make it well suited for early disease detection where disease-associated perturbations are more subtle.
Our research in this area is ongoing. Using the Breath Biopsy OMNI Assay, we have performed parallel untargeted VOC analysis of the same samples collected in the study described above, and we invite you to watch our liver disease webinar to hear more about these findings. Dr Giuseppe Ferrandino presented our research at the online Breath Biopsy Conference in November 2020 as part of the session on breath research for liver diseases, where he talked about developing limonene as an EVOC Probe. For more on this, and other applications of Breath Biopsy, download Breath Biopsy: The Complete Guide.
References
- Fuccilo S, Rudolph B. (2015) Nonalcoholic fatty liver disease. Pediatrics in Review. 36(5):198–206. DOI: 10.1542/pir.36-5-198
- Ferrandino et al. (2020) Breath Biopsy Assessment of Liver Disease Using an Exogenous Volatile Organic Compound—Toward Improved Detection of Liver Impairment Clinical and Translational Gastroenterology 11:e00239. DOI: 10.14309/ctg.0000000000000239
- Fernandez de Rio et al. (2015) Volatile Biomarkers in Breath Associated With Liver Cirrhosis — Comparisons of Pre- and Post-liver Transplant Breath Samples EBioMedicine 2(9), p1243-1250, DOI: 10.1016/j.ebiom.2015.07.027