Breath Testing in Gut Health – Present Reality and Future Opportunities
Published on: 5 Jul 2021

Breath testing is a simple non-invasive way to investigate gastrointestinal health, with a wealth of options already available. These include hydrogen and methane breath testing (HMBT) for conditions such as small intestinal bacterial overgrowth (SIBO) or lactose or fructose malabsorption along with breath tests specifically for Helicobacter pylori and the assessment of gastric emptying using stable 13C. These tests are all currently used at The Functional Gut Clinic to help patients get diagnoses for their troubling gut problems. However, there are many other volatile organic compounds (VOCs) produced by the gut microbiota that could be collected on breath and measured to gain further insight into a patient’s gut health.
This blog post will look at the current breath tests used at The Functional Gut Clinic, other compounds that could be detected on breath with the help of Owlstone Medical’s Breath Biopsy® technology, and how this could help change the landscape of digestive health in the future.
History of Non-invasive Gastrointestinal Biomarker Research
Current breath tests offered in gastrointestinal health
HMBT
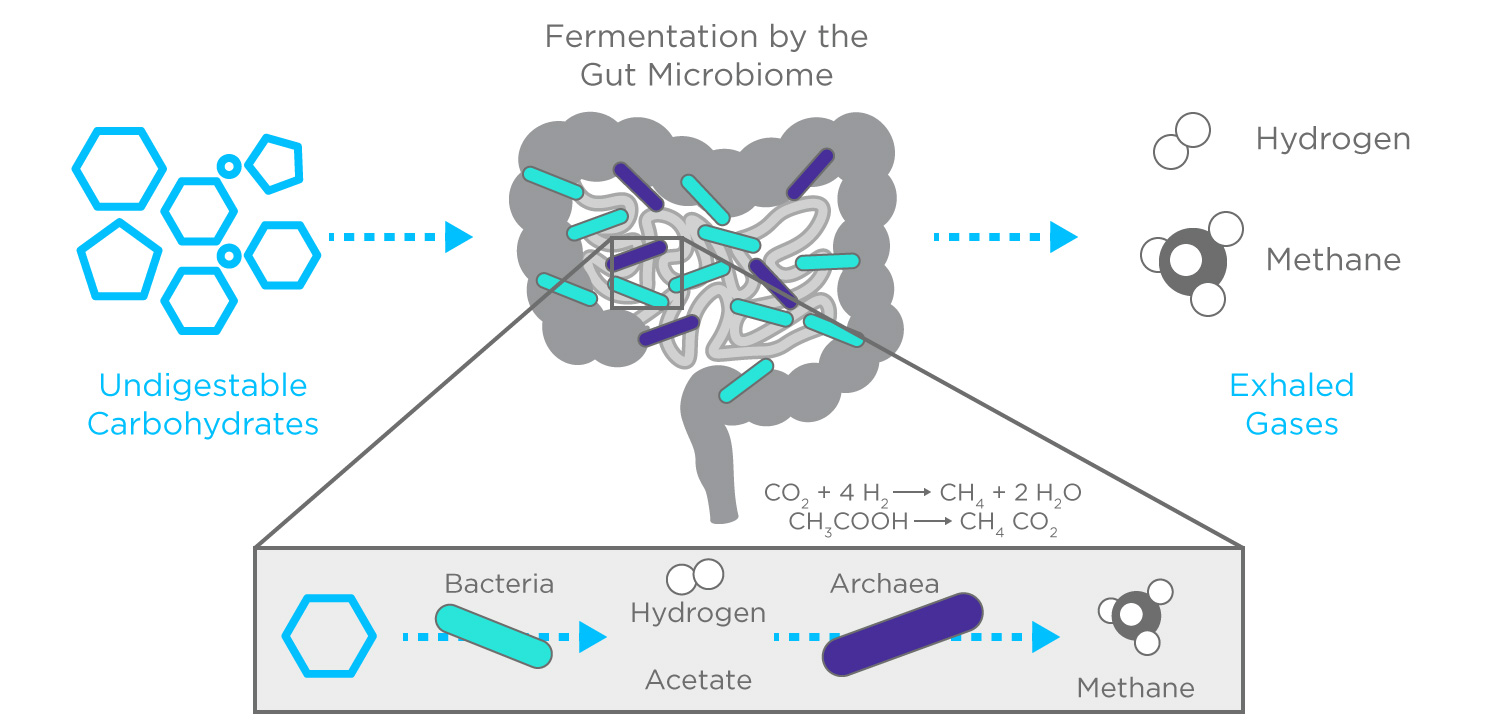
Hydrogen and methane breath testing can be used for the diagnosis of SIBO and food intolerance. SIBO is characterized by bacteria from the colon, which is healthy and plays an important role in digestion, overgrowing in the small bowel. In patients with SIBO, bacterial overgrowth commonly causes an increase in hydrogen gas on breath which can be measured over a period of time in response to the ingestion of a sugar substrate (lactulose or glucose) for a diagnosis.
Lactose (common in dairy) and fructose (common in fruits) breath testing looks to see if an individual has a problem with absorbing lactose or fructose sugar and works on the assumption that gas production following the consumption of these sugars indicates poor absorption as a consequence of fermentation of the sugar by bacteria in the colon.
HMBT is a great way for patients with gastrointestinal symptoms to help understand and control their symptoms. The Functional Gut Clinic provides interpretation by qualified clinical scientists and physiologists and correlates breath gas production with symptoms during the test to support a patient’s diagnosis, ensuring they get the correct diagnosis.
Stable 13C breath testing
Helicobacter pylori is a spiral shaped gram-negative bacterium that can cause stomach ulcers and if left untreated increases the risk of developing stomach cancer. H.pylori can be detected via urea breath testing using 13C urea with orange juice or citric acid. The orange juice/citric acid causes the duodenal sphincter to close to contain the stomach contents. H.pylori survives by excreting urease enzyme which breaks down 13C urea into 13C ammonia and 13C carbon dioxide. The 13C carbon dioxide is then exhaled and collected in end tidal breath samples. High levels of 13C in the breath indicates that there is urease, produced by H.pylori, present in the stomach1.
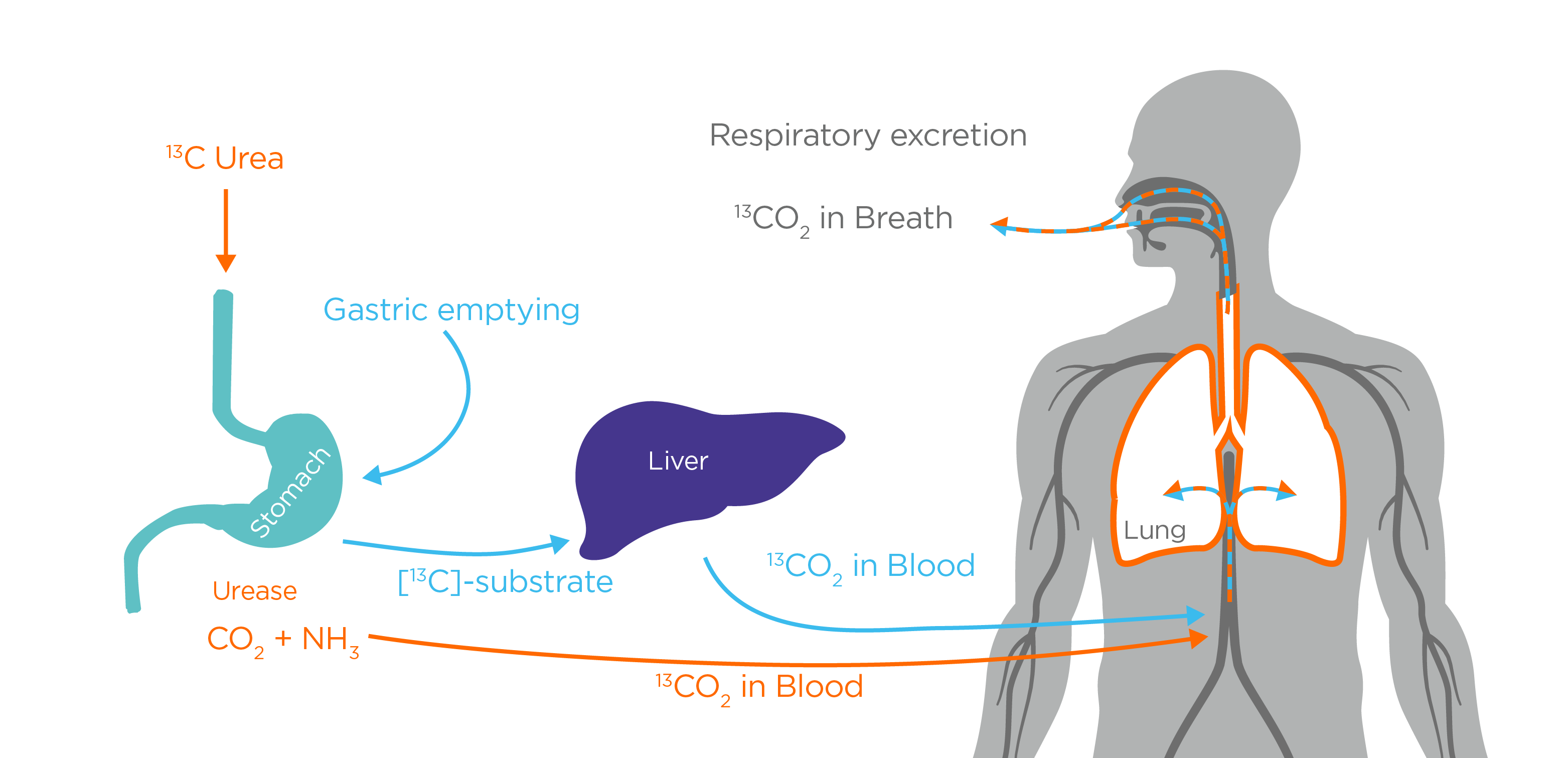
Breath testing to assess gastric emptying is useful to assess for functional dyspepsia and gastroparesis. The gastric emptying test involves the patient eating a solid (egg sandwich) or semi-solid (porridge) test meal, which contains 13C sodium octanoate or 13C sodium acetate respectively3. 13C gastric emptying studies work on the metabolic principle that 13C sodium octanoate and 13C sodium acetate are absorbed in the small intestine, then catabolised by the liver and enter the bicarbonate pool. Approximately 50% of the 13C carbon is exhaled on breath4. The rate limiting step is the stomach emptying speed, allowing the breath test to non-invasively assess gastric emptying5.
ABOUT H. pylori testing about gastric emptying testing
The use of VOCs in the assessment of gastrointestinal health
In gut health one of the main limitations of current breath testing is that tests are constrained to detecting hydrogen, methane and 13CO2, despite the diversity of compounds on breath that are produced by cells, metabolic processes and the gut microbiota. One good example of this is hydrogen sulphide (H2S). High levels of H2S produced by the microbiota have been associated with destabilising the intestinal protective layer and mucosal inflammation6. Current HMBT technology cannot detect SIBO in non-hydrogen producers, and it therefore goes undiagnosed in those that are predominantly H2S producers, which is associated with diarrhoea7.
H2S isn’t the only compound produced by the gastrointestinal microbiota that there is currently no standard breath test for. There are over 1,000 volatile organic compounds (VOCs) that can be detected on breath. These consist of endogenous VOCs from physiological and pathological mechanisms in the body, along with exogenous VOCs which are based upon an individual’s diet, medication and their microbiome.
Non-invasive Biomarkers for Gastrointestinal Diseases
Short chain fatty acids (SCFAs) are one particular type of VOC that are highly abundant in the gastrointestinal tract. They are produced by the microbiota, but little is known about their function. The three SCFAs acetate, propionate and butyrate, make up 90-95% of the SCFAs produced in the colon8, and are known to be beneficial for physiological functions in the gut for example with maintaining the colonic epithelium and influencing colonic motility, blood flow and nutrient absorption9,10.
An important area of current research within digestive health is the ongoing efforts to understand how SCFA production is involved in gastro-oesophageal reflux by causing the stomach to relax and increase air volume11. Other areas of interest are how the increase in butyric and pentanoic acid is implicated in oesophagogastric cancer12, the use of propan-1-ol for monitoring inflammatory bowel diseases (IBD) and 1-methyl-4-propan-2-ylcyclohexa-1,4,-diene as a biomarker for the diagnosis of irritable bowel syndrome (IBS)13. However, this is barely scratching the surface in the potential role of VOCs in gut health. Using VOCs in digestive health could allow us to develop an understanding of the VOC signatures produced by different species in the microbiota and the VOCs which the body itself produces that indicate responses to microbiome metabolism (e.g. inflammation in IBD). This knowledge could be applied via breath tests to help phenotype diseases, predict optimal treatment outcomes and better understand how treatments actually work.
The future of breath testing for gut health
Current breath testing allows for the assessment of gastric emptying, H.pylori infection, SIBO and lactose and fructose malabsorption. By working in partnership with Owlstone Medical, The Functional Gut Clinic are hoping to identify new breath biomarkers that allow for a new generation of non-invasive diagnostic tests for gastrointestinal diseases. Using our existing testing methods many compounds that we know are on breath, such as hydrogen sulphide and short chain fatty acids, cannot be easily detected, so developing new methods to detect these VOCs will allow us to increase the availability of tests that accurately assess gut function and correctly predict which patients will respond well to different treatments.
The small intestine is notoriously difficult to study due to its location, not being reached by either endoscopy or colonoscopy. New VOC-based techniques would be of particular benefit to understanding SIBO and phenotyping bacterial overgrowth, based on the types of bacteria present and the VOC profile produced. This could help us to understand why in some individuals SIBO returns quickly following antibiotic treatment and becomes challenging to eradicate. It may also offer us the opportunity to develop a more precision based medicine approach to treatment of gastrointestinal conditions.
You can find out more about the ideas discussed in this blog in our webinar ‘How Breath Biopsy® is Set to Transform Digestive Health Testing’ with Dr Anthony Hobson, Clinical Director and Senior Clinical GI Scientist at the Functional Gut Clinic. You can also browse all our breath testing for digestive health resources on our Gastrointestinal Diseases hub.
Watch the webinar Visit our Gastrointestinal Diseases Hub
References
- Berger A. (2002) Helicobacter pylori breath tests BMJ, 25, 324(7348):1263. DOI: 10.1136/bmj.324.7348.1263
- Graham et al. (2018) Helicobacter pylori urease for diagnosis of Helicobacter pylori infection: A mini review Journal of Advanced Research, 1;13:51–7 DOI: 10.1016%2Fj.jare.2018.01.006
- Sanaka et al. (2010) Stable isotope breath tests for assessing gastric emptying: A comprehensive review J Smooth Muscle Res, 46(6):267–80. DOI: 10.1540/jsmr.46.267
- Sanaka et al. (2008) Retention, Fixation, and Loss of the [13C] Label: A Review for the Understanding of Gastric Emptying Breath Tests Dig Dis Sci, 29;53(7):1747. DOI: 10.1007/s10620-007-0103-z
- Seahorse Laboratories (2016) 13C-Breath Tests for the Assessment of Specific Enzymatic and Metabolic Functions in vivo, Application Brochure
- Blachier et al. (2020) Production of hydrogen sulfide by the intestinal microbiota and epithelial cells and consequences for the colonic and rectal mucosa. AJP – Gastrointestinal and Liver Physiology [Internet]. [cited 2021 May 25]
- Banik et al. (2016) Hydrogen sulphide in exhaled breath: a potential biomarker for small intestinal bacterial overgrowth in IBS J Breath Res 10;10(2):026010. DOI: 10.1088/1752-7155/10/2/026010
- Lee et al. (2021) Analyses of short-chain fatty acids and exhaled breath volatiles in dietary intervention trials for metabolic diseases Exp Biol Med (Maywood) 1;246(7):778–89. DOI: 10.1177/1535370220979952
- Morrison et al. (2016) Formation of short chain fatty acids by the gut microbiota and their impact on human metabolism Gut Microbes 3;7(3):189–200. DOI: 10.1080/19490976.2015.1134082
- Tan et al. (2014) The role of short-chain fatty acids in health and disease Adv Immunol 121:91–119. DOI: 10.1016/b978-0-12-800100-4.00003-9
- Ropert et al. (1996) Colonic fermentation and proximal gastric tone in humans Gastroenterology 111(2):289–96. DOI: 10.1053/gast.1996.v111.pm8690193
- Adam et al. (2019) Mass-Spectrometry Analysis of Mixed-Breath, Isolated-Bronchial-Breath, and Gastric-Endoluminal-Air Volatile Fatty Acids in Esophagogastric Cancer Anal Chem 5;91(5):3740–6. DOI: 10.1021/acs.analchem.9b00148
- Malderen et al. (2020) Volatomics in inflammatory bowel disease and irritable bowel syndrome EBioMedicine 54:102725 DOI: 10.1016/j.ebiom.2020.102725
