A Brief History of Non-invasive Gastrointestinal Biomarker Research
Published on: 24 Mar 2021
Non-invasive testing for gastrointestinal (GI) illnesses is not a new area of research but it still holds a lot of potential to advance GI medicine and to help millions of people to find relief from chronic symptoms that can severely affect their quality of life. Progress in the field has been led by improvements in technology, and a wave of studies over recent years means that non-invasive breath testing is set to become a more widespread component of GI diagnosis and treatment.
In a previous blog we presented the main reasons why non-invasive breath tests offer such value for the detection and treatment of GI diseases. Here we look at the existing research evidence and the technology that could enable a wider range of non-invasive biomarkers to become valuable clinical tools for GI diagnosis and treatment.
The Beginnings of Non-Invasive GI Biomarkers
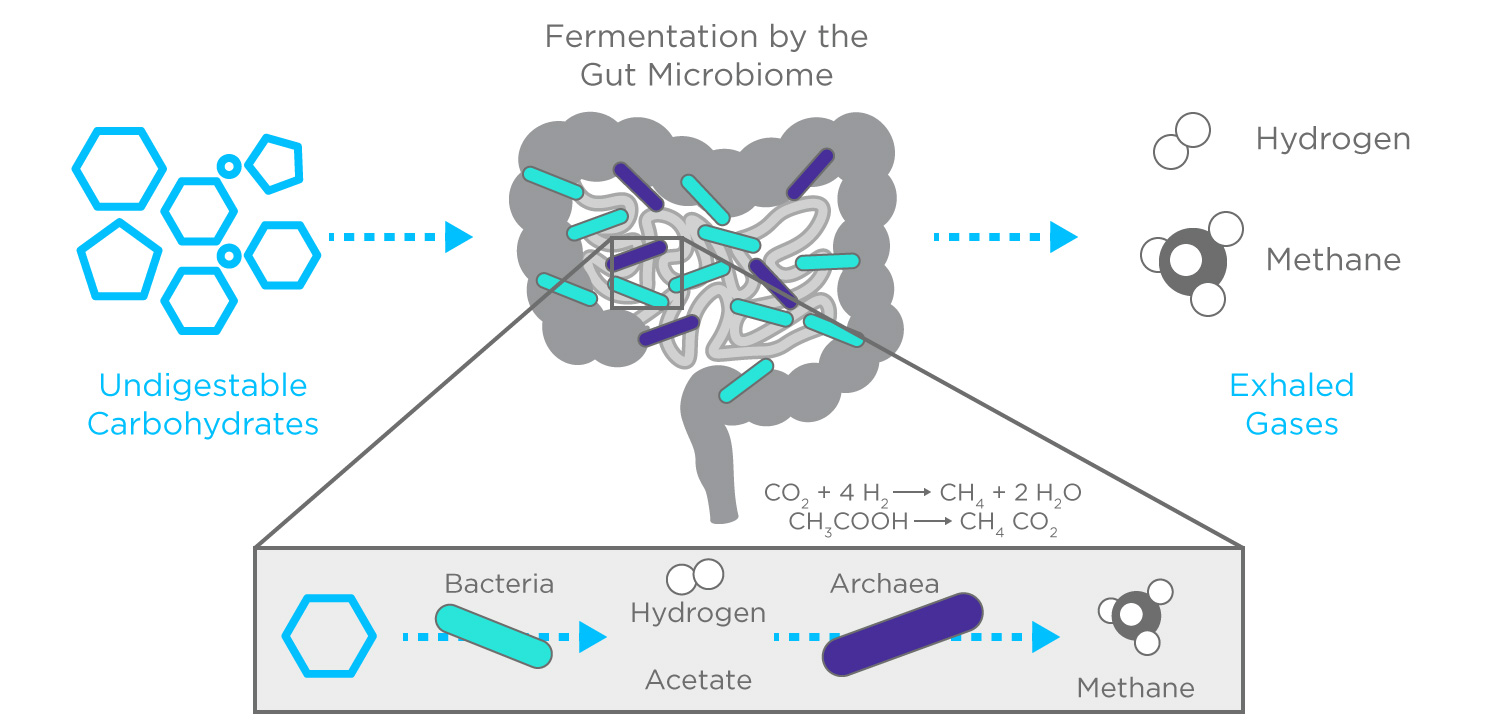
Hydrogen on breath is perhaps the most well-established non-invasive biomarker of GI diseases and has a history dating back as far as the 1970s.1 Early studies focused on lactose malabsorption but hydrogen is useful in a number of GI conditions that involve altered bacterial fermentation, including other carbohydrate intolerances, intestinal transit issues, small intestinal bacterial overgrowth (SIBO)2. Bacterial fermentation produces hydrogen which is absorbed by the blood and detected on breath. Early studies also examined isotope labelled carbon (14C and 13C), which can be detected on breath as labelled CO2, however the difficulties and cost of creating isotope labelled substrates has limited the utility of tests based on these labels.
Volatile organic compounds (VOCs) are a diverse group of chemicals with great potential as non-invasive biomarkers, which can be detected and analyzed on breath, as well as from urine and feces. Key early work on VOCs in biological samples also started in the 70s with Linus Pauling and colleagues.3,4 But the relative complexity of reliably collecting and analyzing the mixture of hundreds of VOCs in these samples has posed a significant research challenge.
Discovering VOC Biomarkers of GI Diseases
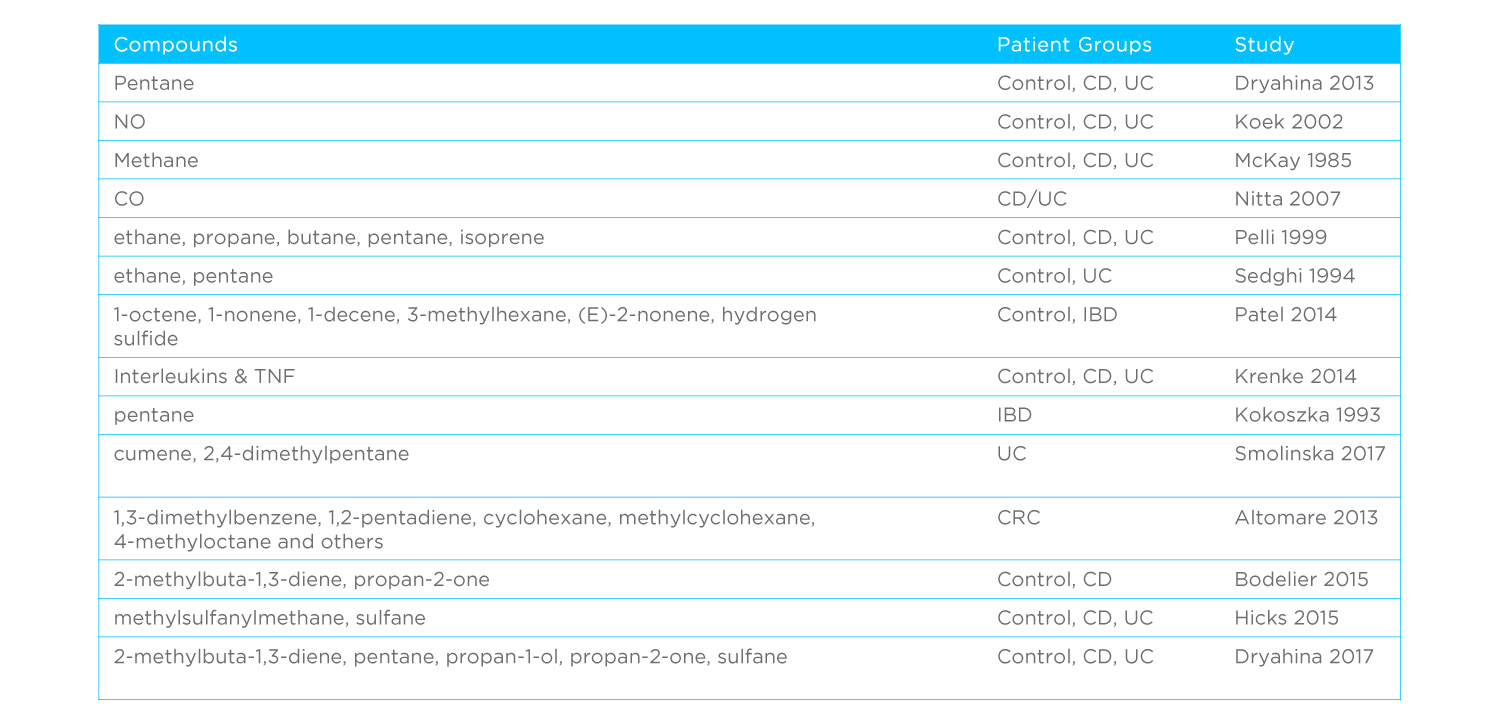
Prior to 2010, a small number of pioneering studies looked at VOCs in GI illnesses, with a particular focus on inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS). Technical limitations meant that these studies typically focused on specific compounds. In one of the earliest studies, Kokoszka et al.5 examined pentane on breath, while a 1999 study from Pelli et al.6 looked at the range of exhaled alkanes. It’s not until Probert et al.7 in 2004 and Garner et al.8 in 2007 that we start to see untargeted analysis of GI conditions, which initially used headspace VOCs, typically from feces or urine.
The last decade has seen a dramatic increase in studies investigating VOC biomarkers of GI health. As many as 40 studies9,10 have been published providing comparisons of IBS to IBD, different IBD phenotypes and active or remission states, as well as examining various infections and cancer. This growth has been associated with an increased interest in metabolic markers of disease, which has largely resulted from the realization that genetics and genomics alone only provide a partial picture of the complex biological interactions that take place in our bodies and the roles that external factors such as diet and the environment have to play in them. Continuing advances in our abilities to detect, distinguish and identify VOCs in complex samples have also been key to enabling this work.
Notably, we have seen a diversification of methods used for VOC analysis. The early studies relied upon Gas Chromatography (GC), or GC Mass Spectrometry (GC-MS). More recent studies have used techniques including selected ion flow tube mass spectrometry (SIFT-MS)20,22,23, our FAIMS technology24,25,26 and chemical sensor-based eNoses. Several approaches are compared in detail in this review.27 While these new approaches offer some advantages for clinical implementation GC-MS remains the gold standard for the discovery and validation of high-quality non-invasive biomarkers.
Compare biomarker analysis technologies
Technology isn’t all that varies about these studies. Diverse, study groups, analysis pipelines and statistical modelling approaches are also used and sample sizes are often small, lacking in internal validation. As such, while results consistently show that VOCs could be effective GI biomarkers, the inconsistencies between studies have stopped VOCs from making it to clinical applications. A number of compounds have been repeatedly identified across studies, with propan-1-ol being one of the most consistent and pentane also featuring along with a selection of other short chain alkanes and aldehydes.
From these studies, themes emerge; a growing confidence that VOCs can provide relevant and useful insights into GI illnesses, a desire for standardized study and analysis methods to enable comparison and validation of results, and a need for reliable identification of biomarkers that are supported by insights into underlying metabolism.
Non-Invasive GI Biomarkers in the 2020s
So, where do we stand now?
Hydrogen breath tests are a licensed diagnostic tool supported by many healthcare systems, including the NHS in the UK. These have largely been combined with methane detection to enhance the reliability of results. 5-15% of false negatives in hydrogen tests are thought to be due to micro-organisms that favour the production of methane over hydrogen28. As such, combined hydrogen methane breath tests (HMBT) provide a much more reliable result. While hydrogen sensors are relatively widely available, reliable methane sensors have yet to emerge, meaning that most HMBT is done offline using approaches such as GC-MS. This includes at-home HMBT where a patient collects their own breath samples and sends them off for specialist analysis.
VOC breath tests have shown up to 100% accuracy in detecting GI disease phenotypes in small-scale studies29. VOCs also appear to show a particular strength in differentiating IBD from IBS, separating ulcerative colitis from Crohn’s disease as the major forms of IBD, and distinguishing active from remission disease states, something which is currently a key clinical challenge. As shown in our previous blog, we can now also clearly link certain VOCs to bacterial metabolism or inflammation underpinning GI illnesses.
As in many fields, the choice of tools and technologies has been critical to progress in VOC biomarker research for GI diseases. Several methods of biomarker collection from breath, urine and feces have been developed and they have been linked to an equally diverse range of detection and analysis platforms. As a result, to date it has been challenging to draw any meaningful conclusions across studies, this is a consistent message across reviews of the field.
As the leaders in non-invasive breath research, we have worked with leaders from the breath VOC community to develop Breath Biopsy®. By prioritising standardization and reproducibility, we’re able to identify VOCs on breath consistently across studies, allowing us to provide the validation that is needed to move VOC biomarkers for GI illnesses towards clinical application. Our ReCIVA® Breath Sampler has been identified by researchers as an optimal solution for standardized breath sample collection32, and Breath Biopsy uses HRAM mass spectrometry to provide robust, high resolution and high sensitivity detection even for low abundance VOCs.
What’s more, our expertise in FAIMS-based chemical detection, means we are well positioned to develop targeted diagnostic tools that provide a practical solution for the implementation of VOC biomarker tests in the clinic for fast and affordable differential diagnosis and precision medicine treatment of the full range of GI conditions.
Find out more about breath test for GI from Anthony Hobson – a leading specialist in GI diagnostics, and in the provision of at-home HMBT – by watching our webinar. If you’d like to know more about integrating Breath Biopsy into your own research then contact our team.
References
- Newcomer et al. (1975) Prospective Comparison of Indirect Methods for Detecting Lactase Deficiency N. Engl. J. Med. 293, 1232–1236 DOI: 10.1056/NEJM197512112932405
- Rezaie et al. (2017) Hydrogen and Methane-Based Breath Testing in Gastrointestinal Disorders: The North American Consensus Am. J. Gastroenterol. 112:775-784 DOI: 10.1038/ajg.2017.46
- Pauling et al. (1971) Quantitative analysis of urine vapor and breath by gas-liquid partition chromatography Proc. Natl. Acad. Sci. U. S. A. 68, 2374–2376 DOI: 10.1073/pnas.68.10.2374
- Teranishi et al. (1972) Gas chromatography of volatiles from breath and urine Anal.Chem. 44, 18–20 DOI: 10.1021/ac60309a012
- Kokoszka et al. (1993) Determination of inflammatory bowel disease activity by breath pentane analysis Dis Colon Rectum 36, 597–601 DOI: 10.1007/BF02049868
- Pelli et al. (1999) Breath alkanes determination in ulcerative colitis and Crohn’s disease Dis. Colon Rectum 42, 71–6 DOI: 10.1007/BF02235186
- Probert et al. (2004) A novel method for rapidly diagnosing the causes of diarrhoea Gut. 53, 58-61 DOI: 10.1136/gut.53.1.58
- Garner et al. (2007) Volatile organic compounds from feces and their potential for diagnosis of gastrointestinal disease The FASEB Journal 21, 1675-88 DOI: 10.1096/fj.06-6927com
- Van Malderen et al. (2020) Volatomics in inflammatory bowel disease and irritable bowel syndrome EBioMedicine 54, 102725 DOI: 10.1016/j.ebiom.2020.102725
- Wilson (2018) Application of Electronic-Nose Technologies and VOC-Biomarkers for the Noninvasive Early Diagnosis of Gastrointestinal Diseases Sensors 18, 2613 DOI: 10.3390/s18082613
- Dryahina et al. (2013) Quantification of pentane in exhaled breath, a potential biomarker of bowel disease, using selected ion flow tube mass spectrometry Rapid Commun. Mass Spectrom. 27, 1983–92 DOI: 10.1002/rcm.6660
- Koek et al. (2002) Activity related increase of exhaled nitric oxide in Crohn’s disease and ulcerative colitis: a manifestation of systemic involvement? Respir. Med. 96, 530–5 DOI: 10.1053/rmed.2002.1312
- McKay et al. (1985) Methane excretion in man – a study of breath, flatus, and faeces Gut 26, 69–74 DOI: 10.1136/gut.26.1.69
- Nitta et al. (2007) Exhaled carbon monoxide concentration is not elevated in patients with inflammatory bowel disease Clin. Exp. Med. 7, 77–81 DOI: 10.1007/s10238-007-0129-8
- Sedghi et al. (1994) Elevated breath ethane levels in active ulcerative colitis: evidence for excessive lipid peroxidation Am. J. Gastroenterol. 89, 2217–21 https://pubmed.ncbi.nlm.nih.gov/7977245/
- Patel et al. (2014) Metabolomic analysis of breath volatile organic compounds reveals unique breathprints in children with inflammatory bowel disease: a pilot study Aliment Pharmacol Ther. 40, 498-507 DOI: 10.1111/apt.12861
- Krenke et al. (2014) Inflammatory cytokines in exhaled breath condensate in children with inflammatory bowel diseases. Pediatr. Pulmonol. 49, 1190–5 DOI: 10.1002/ppul.22953
- Smolinska et al. (2017) The potential of volatile organic compounds for the detection of active disease in patients with ulcerative colitis Aliment Pharmacol. Ther. 45, 1244–54 DOI: 10.1111/apt.14004
- Bodelier et al. (2015) Volatile organic compounds in exhaled air as novel marker for disease activity in Crohn’s disease: a metabolomic approach Inflamm. Bowel Dis. 21, 1776–85 DOI: 10.1097/MIB.0000000000000436
- Hicks et al. (2015) Analysis of Exhaled Breath Volatile Organic Compounds in Inflammatory Bowel Disease: A Pilot Study Journal of Crohn’s and Colitis 9, 731–737, DOI: 10.1093/ecco-jcc/jjv102
- Dryahina et al. (2017) Pentane and other volatile organic compounds, including carboxylic acids, in the exhaled breath of patients with Crohn’s disease and ulcerative colitis J. Breath Res. 12, 016002 DOI: 10.1088/1752-7163/aa8468
- Rieder et al. (2016) A Distinct Colon-Derived Breath Metabolome is Associated with Inflammatory Bowel Disease, but not its Complications Clinical and Translational Gastroenterology 7, e201 DOI: 10.1038/ctg.2016.57
- Arasaradnam et al. (2014) Next generation diagnostic modalities in gastroenterology – gas phase volatile compound biomarker detection Aliment Pharmacol Ther. 39, 780–789 DOI: 10.1111/apt.12657
- Arasaradnam et al. (2014) Differentiating Coeliac Disease from Irritable Bowel Syndrome by Urinary Volatile Organic Compound Analysis – A Pilot Study PLoS ONE 9, e107312 DOI: 10.1371/journal.pone.0107312
- Arasaradnam et al. (2015) Non-invasive exhaled volatile organic biomarker analysis to detect inflammatory bowel disease (IBD) Dig. Liver Dis. DOI: 10.1016/j.dld.2015.10.013
- Tomasz Majchrzak et al. (2018) Sample preparation and recent trends in volatolomics for diagnosing gastrointestinal diseases Trends in Analytical Chemistry 108, 38–49 DOI: 10.1016/j.trac.2018.08.020
- de Lacy Costello et al. (2013) The importance of methane breath testing: a review. J. Breath Res. 7, 024001. DOI: 10.1088/1752-7155/7/2/024001
- Aggio et al. (2017) Irritable bowel syndrome and active inflammatory bowel disease diagnosed by faecal gas analysis. Aliment Pharmacol Ther. 45, 82–90. DOI: 10.1111/apt.13822
- Azim et al. (2019) Exhaled volatile organic compounds in adult asthma: a systematic review. Eur. Respir. J. 54, 1900056 DOI: 10.1183/13993003.00056-2019