Assessing inflammation in stroke patients
Breath VOCs appear to track established plasma biomarkers and correlate with metabolic pathways
| Publication information: Ahmed, W. et al. Breath and plasma metabolomics to assess inflammation in acute stroke (2021) Sci Rep 11, 21949. DOI: 10.1038/s41598-021-01268-5
Disease Area: Stroke, Ischemic disease Application: Patient monitoring Sample medium: Breath, Plasma Analysis approach: TD-GC-ToF-MS Summary:
|
Strokes are the second largest cause of death globally in addition to the most common cause of neurological disability. According to the Centers for Disease Control and Prevention, in the US alone, there are around 800,000 strokes each year – around 1 every 40 seconds. The cognitive, behavioral and mobility issues experienced by many stroke patients can make ongoing health monitoring challenging, and many methods are unsuitable for use with these patients. Yet, monitoring can be extremely important, as patients in recovery from a stroke can be vulnerable to complications. For example, around 1 in 7 develop pneumonia, which is associated with significantly worse clinical outcomes. There is great clinical need for new tests that can monitor stroke patients during recovery and predict complication risks and long-term prognosis inexpensively and non-invasively – breath-based biomarkers could hold the solution.
Both ischemic strokes (the most common), resulting from reduced blood flow to the brain, and strokes resulting from intracerebral hemorrhages (the most deadly), induce an inflammatory response in the body when they occur. Markers of this response have been identified in blood samples and could help to predict complication, but collecting samples is invasive, and not suitable for regular monitoring. Many metabolic mechanisms involved in inflammation produce volatile organic compounds (VOCs), alongside other metabolites, that can be collected and analyzed non-invasively in a breath sample. Identifying and measuring these VOCs has been the focus of many other breath studies and represents an exciting opportunity for precision medicine across many disease areas.
Ahmed et al. set out to examine the feasibility of breath sampling and breath monitoring in patients admitted to hospital having suffered an acute stroke. The study aimed to find out whether repeated breath sampling would be well-tolerated by this vulnerable patient group and to analyze how well any potential breath biomarkers correlated with established markers of stroke-associated inflammation, such as those found in blood plasma.
Method
20 patients with either ischemic strokes or intracerebral hemorrhages were recruited into the study and breath was initially collected within 24 hours of initial stroke symptoms. Breath collections were then repeated every two days until either day 15, or discharge from hospital, whichever occurred earlier. Blood plasma samples for analysis were also collected during this timeframe.
Breath samples were analyzed using TD-GC-ToF-MS. Analysis of patient breath samples was targeted to 46 specific VOCs, with the primary focus being on 22 compounds which had previously been suggested as potential biomarkers of inflammation or infection in the literature. The other 24 VOCs were external standards.
Results
Of the 22 breath-based VOCs targeted as part of analysis, two (α-pinene and decanal) exhibited significant variance in samples collected soon after the stroke onset, in comparison to samples collected later.
All 22 breath VOCs were then investigated for correlation with levels of C-reactive protein CRP and interleukin-6 (IL-6), known inflammatory mediators found in the blood plasma samples. Decanal, benzaldehyde and pyridine showed the strongest positive correlation with CRP, while 1,4-dioxane, 2-pentanone and hexane exhibited the strongest negative correlation. Decanal, benzyl alcohol and tetralin correlated most positively with IL-6, and nonane, heptanal and nonanal showed negative correlation. Breath VOCs were also found to correlate highly with other plasma metabolites including alkanes and terpenes – which suggests these plasma metabolites may be directly linked to the VOCs measured on breath.
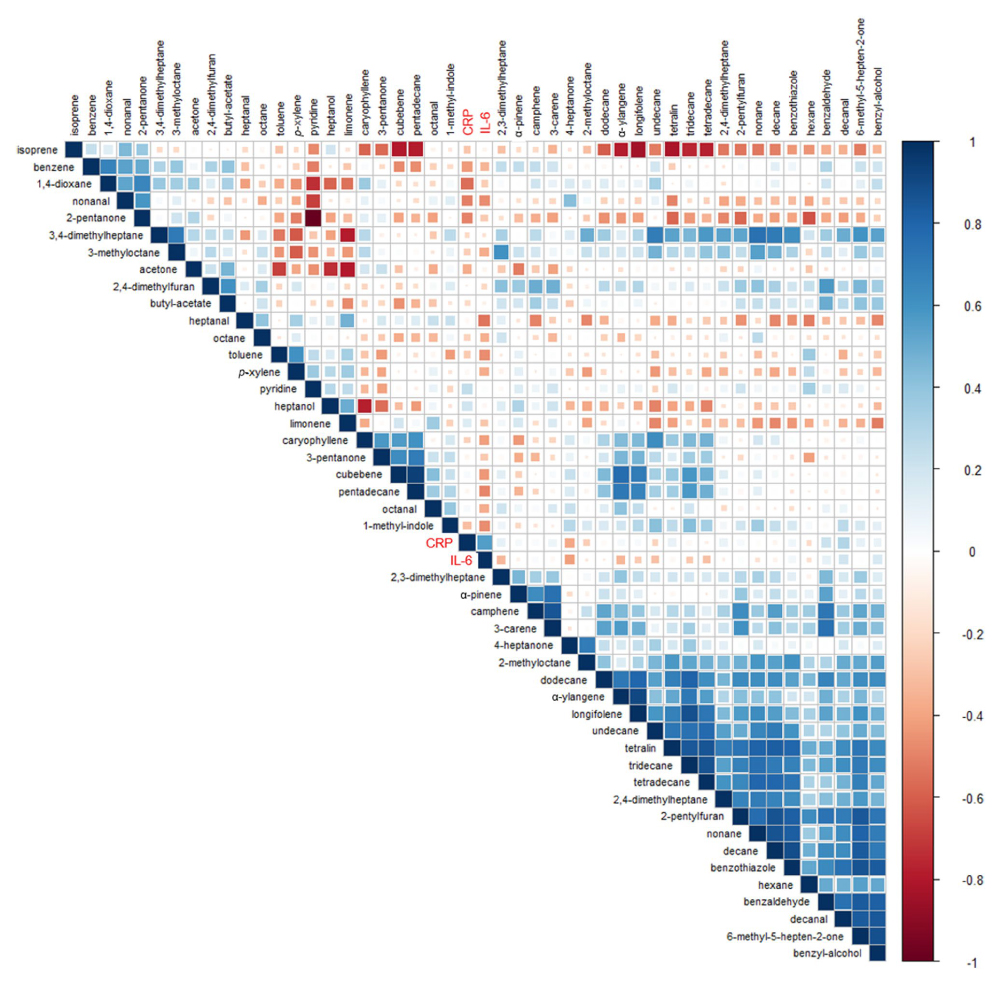
Figure 1: Correlations matrix plot of breath VOCs and inflammatory markers (CRP and IL-6). Each square represents the relationship between the compound above it and the compound to its left. Pearson’s correlation coefficients are shown by colour strength and square size, where 1 is strong positive correlation, -1 is strong negative correlation, and 0 is no correlation.
Conclusions
Of the stroke patients eligible to participate in the study none withdrew due to intolerance of breath sampling. All attempts at collecting breath samples were completed successfully. This led Ahmed et al. to conclude ‘recruitment is feasible, and sampling well-tolerated, in dysphagic patients and in patients with moderate or severe stroke, supporting further breath studies in acute stroke’.
Correlation found in this study between VOCs and plasma metabolites has supported the idea that specific VOCs, detectable on breath, are likely to be endogenous products of metabolic processes. This study targeted 22 VOCs that had a previously been linked to inflammation in the literature. Follow up studies, in addition to validating this study’s results, would benefit from taking an untargeted approach, in the search for new biomarkers that may have previously been missed.
No patients in this study developed stroke-associated pneumonia so it wasn’t possible to investigate potential biomarkers for early diagnosis of pneumonia infection. Future studies that want to look into this area would therefore need to significantly increase the study size in order to gather meaningful results. Such a study has the potential to be extremely valuable because of the strong association between pneumonia infection and worse outcomes for stroke patients.
In reference to Owlstone Medical’s ReCIVA Breath Sampler®, Ahmed et al. state ‘The principles underlying our breath sampler have been further developed through the Breathe-Free consortium, and a commercial sampler based on this concept is now available, further facilitating larger scale clinical studies’.
The ReCIVA Breath Sampler is just one part of our industry-leading breath sample collection and analysis platform, Breath Biopsy, that we developed in partnership with our academic and clinical collaborators to provide reliable breath collection and analysis. Get in touch to find out how Breath Biopsy could support your own research study.
FIND OUT MORE ABOUT THE BREATH BIOPSY COLLECTION STATION LET’S TALK
